Prolactin Surgery: What It Is and Why It Matters
When dealing with prolactin surgery, the surgical removal of prolactin‑producing pituitary lesions. Also known as pituitary adenoma resection, it offers a direct way to lower excess prolactin when medication isn’t enough.
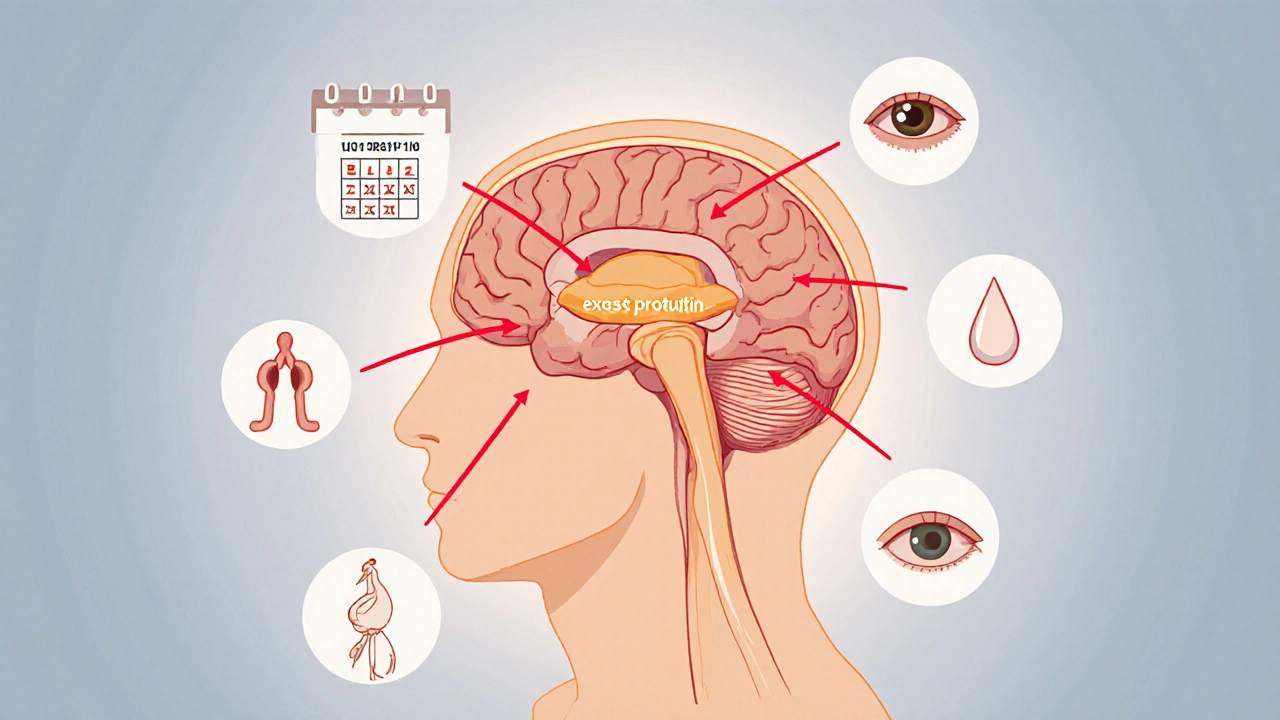
The hormone at the heart of the issue is prolactin, a protein made by the pituitary gland that regulates milk production and influences reproductive function. When a pituitary adenoma, a benign tumor that can overproduce prolactin grows, patients often experience headaches, vision changes, and infertility. Doctors first try dopamine agonists, medications like cabergoline or bromocriptine that shrink the tumor by lowering prolactin output. If the tumor resists medication, causes severe symptoms, or threatens surrounding brain tissue, surgery becomes the recommended option.
When Hormonal Imbalance Pushes Toward Surgery
A broader hormonal imbalance, any disruption in the endocrine system that affects multiple hormones can tip the scale. For example, low testosterone, high cortisol, or thyroid disorders can worsen prolactin‑related symptoms, making the decision for surgery more urgent. Imaging tools like MRI confirm tumor size, while lab tests track prolactin levels before and after any intervention. Understanding how these entities interact helps patients and clinicians choose between continued medication, radiation, or surgical removal. Below you’ll find a curated set of articles that walk through medication comparisons, side‑effect profiles, and step‑by‑step guides on managing the whole endocrine picture around prolactin surgery.
Explore medication and surgery options for hyperprolactinaemia, learn how dopamine agonists work, when surgery is needed, and how to monitor treatment effectively.
Oct, 12 2025