Hyperprolactinaemia Treatment Options: Meds, Surgery & What Works Best
Hyperprolactinaemia Treatment Success Calculator
Estimated Success Rate
0%
Based on clinical evidence from treatment studies
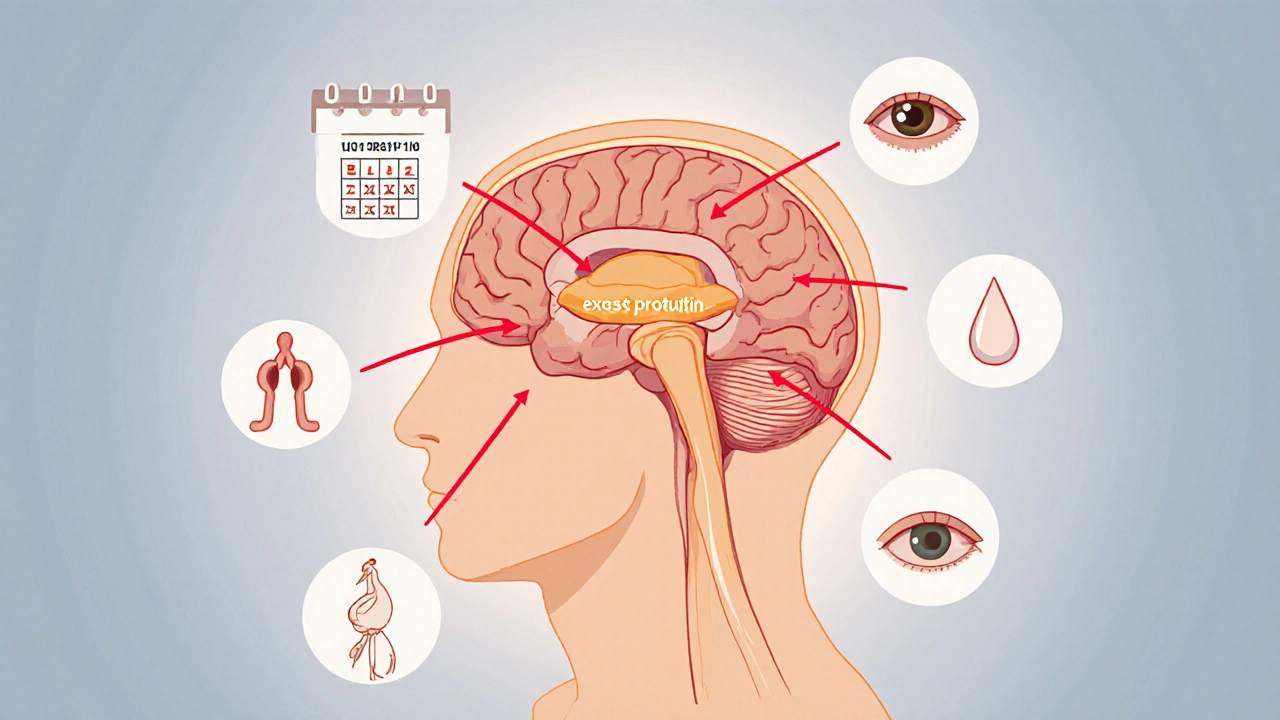
Hyperprolactinaemia is a hormonal disorder where the pituitary gland releases too much prolactin, leading to irregular periods, infertility, unwanted breast milk, and sometimes vision problems.
Key Takeaways
- First‑line treatment is usually a dopamine agonist such as cabergoline or bromocriptine.
- Surgery becomes an option when medication fails, when a large pituitary adenoma causes pressure symptoms, or when drug side‑effects are intolerable.
- Regular monitoring of prolactin level and periodic MRI scans guide therapy adjustments.
- Most patients achieve normal prolactin levels within weeks of starting medication.
- Transsphenoidal surgery has a success rate above 85% for small, well‑localized tumours.
Understanding Hyperprolactinaemia
The condition can stem from a tiny tumour called a pituitary adenoma, certain medications (antipsychotics, anti‑emetics), hypothyroidism, or even stress. When prolactin stays high, the hypothalamic‑pituitary‑gonadal axis gets disrupted, which explains the reproductive symptoms.
Why treat it? Persistent elevation raises the risk of osteoporosis, chronic infertility, and in rare cases, can press on the optic chiasm, causing visual field defects.
Medication Options: Dopamine Agonists
All approved drugs belong to the dopamine agonist class. They mimic dopamine’s inhibitory effect on prolactin secretion.
Bromocriptine
Bromocriptine was the first oral agent. Typical dosing starts at 1.25mg daily, titrated up to 5mg three times a day. It normalizes prolactin in 60‑70% of cases, but the multiple daily doses can cause nausea and fatigue.
Cabergoline
Cabergoline is now the preferred first‑line drug because of its longer half‑life. A common regimen is 0.25‑0.5mg twice weekly, sometimes extending to 1mg per week for resistant cases. Clinical trials show >85% success in restoring normal menstrual cycles and fertility, with fewer gastrointestinal side‑effects than bromocriptine.
Quinagolide
Quinagolide is taken once daily, starting at 50µg and increasing to 300µg. It offers an alternative for patients who cannot tolerate the other two, though long‑term data are more limited.

When Medication Isn’t Enough
About 10‑15% of patients either don’t respond adequately or develop intolerable side‑effects. In those scenarios, surgical removal of the tumour becomes the next logical step.
Transsphenoidal Surgery: What to Expect
Transsphenoidal surgery accesses the pituitary through the nose and sphenoid sinus, avoiding a brain craniotomy. The procedure is usually done under general anaesthesia and lasts 2‑3hours.
Success rates depend on tumour size: microadenomas (<10mm) have a cure rate of 90‑95%, while macroadenomas (10‑40mm) drop to 70‑80%. Post‑op complications are rare but can include temporary diabetes insipidus, CSF leak, or nasal congestion.
Choosing Between Meds and Surgery
Decision factors include:
- Tumour size: Small lesions usually respond well to meds; large compressive tumours may need early surgery.
- Speed of symptom relief: Medication can normalize prolactin within weeks, while surgery offers an immediate drop post‑op.
- Patient preference: Some dislike daily pills; others fear surgery.
- Pregnancy plans: Cabergoline is considered relatively safe, but surgeons often recommend medication before conception.
- Cost and access: In many health systems, meds are covered long‑term, while surgery may require specialist referral and higher upfront expense.

Monitoring & Managing Side Effects
After starting a dopamine agonist, check prolactin level at 4‑6weeks, then every 6‑12months. MRI scans are recommended at baseline and if symptoms worsen.
Common side‑effects:
- Nausea - take meds with food or shift to cabergoline.
- Headache - mild analgesics usually suffice.
- Orthostatic hypotension - stand up slowly, stay hydrated.
For surgical patients, a post‑op endocrine clinic follow‑up within 2weeks checks for hormone deficits and confirms tumour removal via MRI.
Comparison of Dopamine Agonists
| Drug | Typical Dose | Success Rate | Common Side‑effects | Convenience |
|---|---|---|---|---|
| Bromocriptine | 1.25‑5mg 3×/day | 60‑70% | Nausea, fatigue | Multiple daily doses |
| Cabergoline | 0.25‑1mg twice weekly | 85‑90% | Headache, dizziness | Twice‑weekly, easy |
| Quinagolide | 50‑300µg daily | ~70% | GI upset, rash | Once daily |
Practical Checklist Before Starting Treatment
- Confirm diagnosis with serum prolactin and a baseline MRI of the pituitary.
- Rule out secondary causes (hypothyroidism, medication-induced).
- Discuss fertility goals and pregnancy timing.
- Choose a dopamine agonist based on side‑effect profile and dosing convenience.
- Set follow‑up dates: 4‑week labs, 6‑month MRI, then annual review.
- If prolactin remains >2× upper limit after 6months of maximized dose, refer to a neurosurgeon for possible transsphenoidal surgery.
Frequently Asked Questions
Can hyperprolactinaemia resolve without medication?
Rarely. Most cases are linked to a tumour or a persistent physiological trigger, so medication or surgery is needed to bring prolactin back to normal.
Is it safe to become pregnant while on cabergoline?
Studies show low‑dose cabergoline does not increase birth defects. Many clinicians keep women on the lowest effective dose until conception, then pause the medication under specialist guidance.
How long does it take for prolactin to normalize after surgery?
Most patients see a dramatic drop within 24‑48hours. Full hormonal stabilization is usually confirmed at the 6‑week post‑op visit.
What are the long‑term risks of untreated hyperprolactinaemia?
Chronic high prolactin can lead to bone density loss, persistent infertility, and, if the tumour grows, possible vision loss from optic chiasm compression.
Do all patients need regular MRI scans?
If medication fully controls prolactin and the tumour is small, yearly MRI is often unnecessary. However, any rise in prolactin or new symptoms warrants repeat imaging.

Nikita Warner
October 12, 2025 AT 03:29Hyperprolactinaemia is most often managed initially with dopamine agonists such as cabergoline or bromocriptine, which suppress prolactin secretion in the majority of patients. Cabergoline’s twice‑weekly dosing schedule tends to be better tolerated, while bromocriptine may require multiple daily doses and can cause nausea. If medication fails to normalize prolactin levels after an adequate trial, or if the adenoma is large enough to cause visual field defects, transsphenoidal surgery becomes the next logical step. Regular follow‑up includes serum prolactin measurements and periodic MRI to monitor tumour size. The choice between medical and surgical therapy should be individualized based on tumour characteristics, side‑effect profile, and patient preference.
Liam Mahoney
October 13, 2025 AT 03:46Honestly, people who ignore the importance of adherence to dopamine agonist therapy are just asking for trouble; you cant expect miracles if you skip doses or quit because of a little nausea. The meds are proven, the data is solid, and the side‑effects are manageable with proper titration. Stop making excuses and talk to your endocrinologist about dose adjustments instead of throwing away a proven treatment. It's morally irresponsible to disregard such a simple, life‑changing intervention.
Eric Appiah Tano
October 14, 2025 AT 02:00Great rundown! If you’re just starting out, remember that the first few weeks can feel a bit rough as the body adjusts, but most folks see prolactin levels tumble quickly. Keep a symptom diary-you’ll be surprised how much clarity a simple log brings when you discuss progress with your doctor. Also, don’t forget about lifestyle tweaks like stress reduction; they can boost the effectiveness of the medication.
Justin Ornellas
October 15, 2025 AT 00:13Allow me to clarify the pharmacodynamics at play: dopamine agonists bind to D2 receptors on lactotroph cells, effectively turning off prolactin secretion. The superiority of cabergoline rests on its higher receptor affinity and longer half‑life, which translates into fewer daily doses. While surgery offers a definitive solution for macroadenomas, it carries risks that medical therapy sidesteps in most microadenoma cases. Thus, the evidence hierarchy indisputably favors a trial of cabergoline before contemplating an operative approach.
Jonathan Lindsey
October 15, 2025 AT 22:26Ah, the sheer delight of navigating hyperprolactinaemia treatment-truly the pinnacle of modern endocrinology’s triumphs. One begins with the blessed elixir of cabergoline, a drug that, if taken dutifully, reduces prolactin levels faster than a teenager can post a selfie. The dosing schedule, a mere twice‑weekly ritual, feels almost poetic compared to the drudgery of three‑times‑daily bromocriptine. Yet, for those who relish complexity, bromocriptine offers nausea and fatigue as complimentary side‑effects. Quinagolide, the oft‑overlooked understudy, steps onto the stage with a once‑daily regimen, though its long‑term dossier reads like an unfinished novel. Should any of these pharmacologic overtures fail, the spotlight shifts to the operating theatre, where transsphenoidal surgery promises a swift, albeit invasive, resolution. Surgeons navigate the cavernous sinus with the finesse of a seasoned sculptor, excising the adenoma while sparing the surrounding neural architecture. Success rates above eighty‑five percent for microadenomas sound reassuring, until one remembers that macroadenomas still flirt with suboptimal outcomes. Post‑operative monitoring, of course, mandates serial prolactin measurements and neuro‑ophthalmic examinations-because nothing says “peace of mind” like another lab draw. Patients are encouraged to maintain a calcium‑rich diet to combat potential osteopenia, a reminder that the journey never truly ends. Moreover, the specter of tumor recurrence looms, necessitating periodic MRI scans that cost more than a weekend getaway. Insurance paperwork, meanwhile, becomes an obstacle course worthy of an Olympic event. Yet, through all this, the patient emerges victorious, armed with normalized hormone levels and a renewed sense of reproductive possibility. In summary, the therapeutic algorithm is a masterclass in patience, perseverance, and occasional peripheral vision loss. So, dear readers, may your prolactin descend, your scans be clear, and your sarcasm remain ever abundant.
Gary Giang
October 16, 2025 AT 20:40That color‑coded calculator is pure gold.
steve wowiling
October 17, 2025 AT 18:53It’s almost poetic how the pituitary decides to throw a hormonal tantrum, turning your life into a tragic opera where prolactin is the overzealous soprano. When the meds finally hush that diva, you feel like you’ve reclaimed the stage, only to realize the real drama was the endless doctor visits. The whole saga reminds us that even the smallest gland can script an epic.
Warren Workman
October 18, 2025 AT 17:06While the mainstream consensus lauds cabergoline as the gold standard, it’s worth noting that the pharmacokinetic model overlooks inter‑individual variability in hepatic CYP2D6 expression, which can dramatically attenuate drug efficacy. Moreover, the surgical literature often underreports micro‑vascular complications due to selective reporting bias, casting doubt on the advertised >85% remission rates. Therefore, a rational skeptic must question whether the prevailing treatment algorithm truly optimizes patient outcomes or merely reflects industry‑driven inertia.
Shelby Rock
October 19, 2025 AT 15:20i cant help but wonder if the prolactin surge is just our bodies whispering that we are too busy chasing external validation, forgetting the quiet hum of inner balance. maybe the real cure is learning to listen to that hum, but i guess we need a pill for that too.
Alex Iosa
October 20, 2025 AT 13:33It is evident that the pharmaceutical narrative surrounding dopamine agonists has been meticulously curated by vested interests seeking to monopolize hormone regulation. The selective citation of favorable clinical trials, while marginalizing dissenting data, suggests a coordinated effort to shape clinical guidelines in a manner that serves economic agendas rather than patient autonomy. Consequently, clinicians should maintain a critical vigilance when endorsing these therapies.
melissa hird
October 21, 2025 AT 11:46Bravo, dear authors, for assembling a spreadsheet that rivals the complexity of a NASA flight plan-truly, we’ll all sleep soundly knowing we can click a button and receive a percentage that reassures our existential dread.
Abraham Gayah
October 22, 2025 AT 10:00Honestly, if you’ve read anything beyond the surface-level brochure, you’ll know that the nuanced interplay of endocrine feedback loops makes this whole “just take a pill” narrative look like child’s play.
rajendra kanoujiya
October 23, 2025 AT 08:13Sure, but who says the “nuanced interplay” isn’t just marketing fluff?