Pituitary Adenoma Medication: Guide to Treatment Options
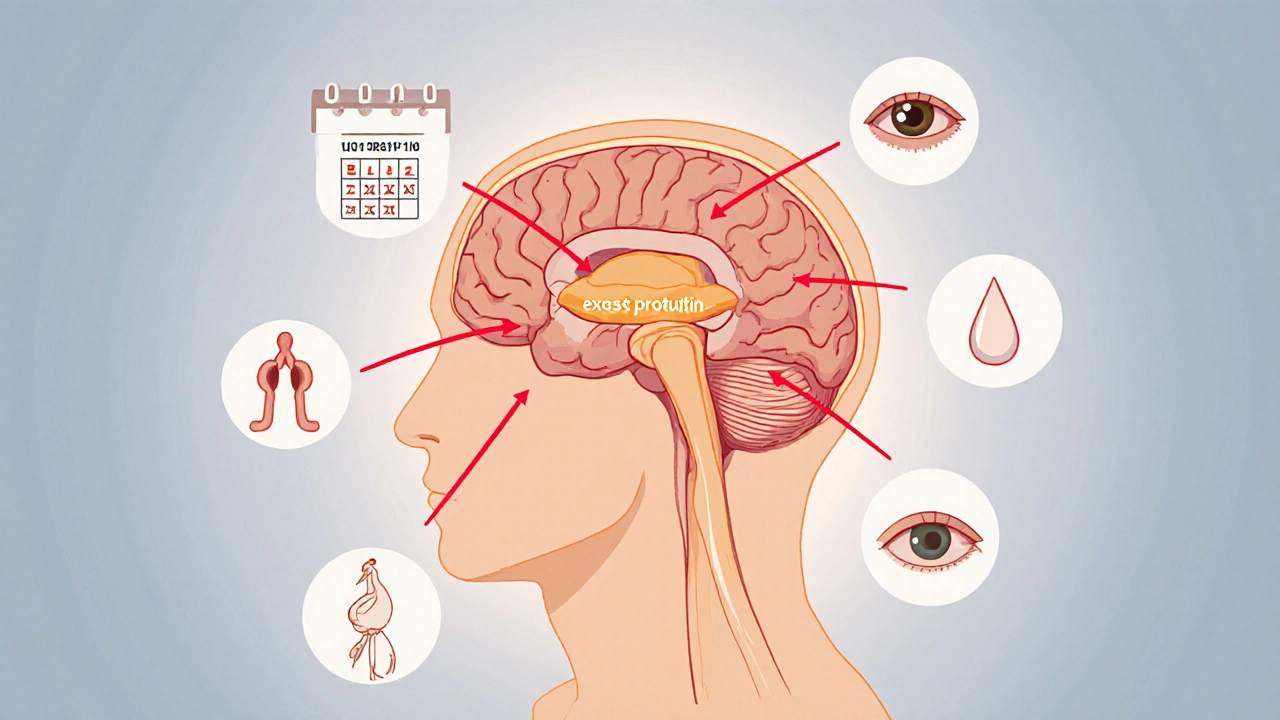
When dealing with Pituitary Adenoma Medication, pharmaceuticals used to control hormone‑secreting or non‑functioning pituitary tumors. Also known as pituitary tumor drugs, it plays a crucial role in shrinking tumors and normalizing hormone levels. The condition itself, Pituitary Adenoma, a benign growth in the pituitary gland that can affect hormone production, often requires a mix of medication, surgery, or radiotherapy. Two drug families dominate the landscape: Dopamine Agonists, agents that lower prolactin by stimulating dopamine receptors and Somatostatin Analogs, compounds that inhibit growth‑hormone release. Together they illustrate how pituitary adenoma medication encompasses targeted hormone control, while the broader treatment plan often requires surgery or radiation to address tumor mass.
Key Medication Classes and How They Work
Dopamine Agonists, such as cabergoline and bromocriptine, act on D2 receptors to suppress excess prolactin and are the first‑line choice for prolactin‑secreting adenomas. They typically lower tumor size by 30‑50% and improve symptoms like galactorrhea and infertility. Somatostatin Analogs, including octreotide and lanreotide, bind to somatostatin receptors, curbing growth‑hormone and IGF‑1 production in acromegaly‑causing adenomas. These drugs can shrink tumors by up to 40% and restore normal metabolic function. For GH‑producing tumors resistant to analogs, GH‑Receptor Antagonists, like pegvisomant, block GH action at peripheral tissues provide an alternative route. Each class carries specific side‑effect profiles—nausea and orthostatic hypotension for dopamine agonists, gallstones and GI upset for somatostatin analogs—so monitoring labs and imaging is vital.
The decision tree for managing a pituitary adenoma often follows this pattern: medication ↔ surgery ↔ radiotherapy. If medication fails to control hormone excess or tumor size, Transsphenoidal Surgery, a minimally invasive approach through the nasal cavity becomes the next step. Post‑operative patients may still need drugs to keep hormone levels in check, especially if residual tumor remains. In cases where surgery isn’t feasible, stereotactic radiosurgery offers precise radiation that can stabilize growth over months. Understanding these connections—how drugs influence hormone secretion, how surgery removes bulk, and how radiotherapy pads the gaps—helps patients and clinicians craft a personalized plan. Below you’ll find a curated list of articles that dive deeper into each medication, compare treatments, and share real‑world tips for navigating pituitary adenoma care.
Explore medication and surgery options for hyperprolactinaemia, learn how dopamine agonists work, when surgery is needed, and how to monitor treatment effectively.
Oct, 12 2025