Opioid Side Effects: What You Need to Know Before Taking Them
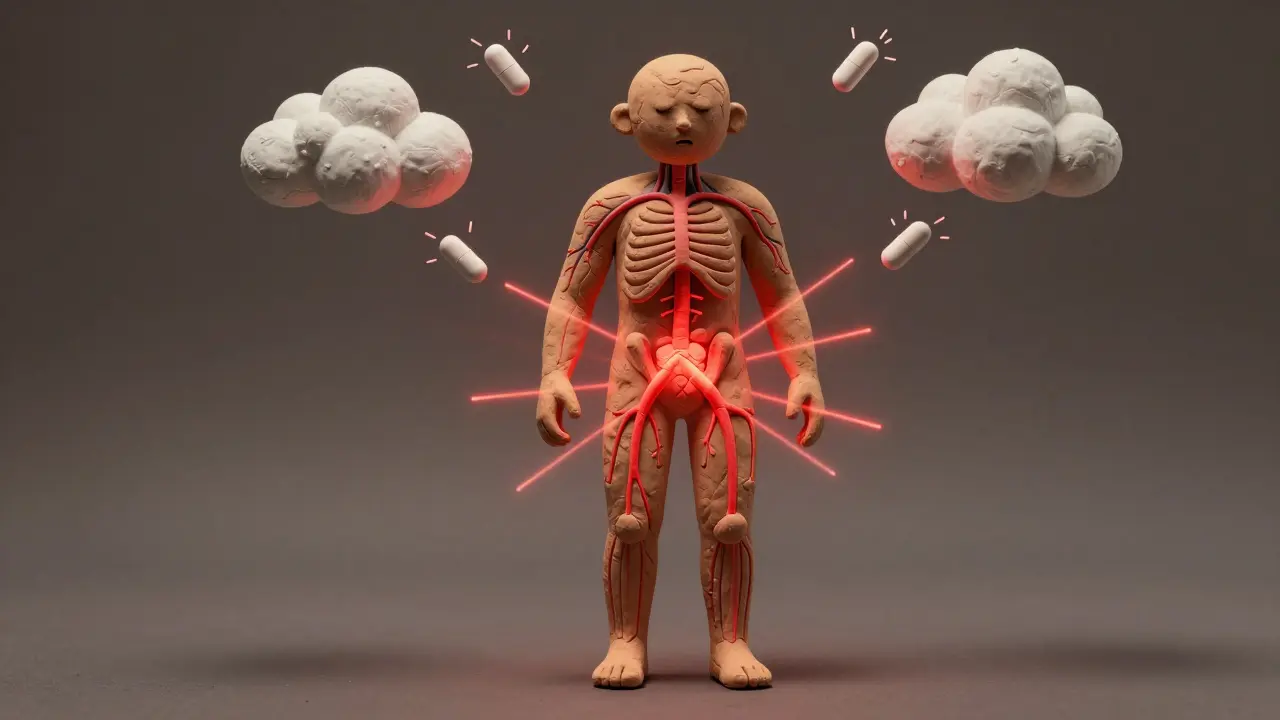
When you take opioids, a class of powerful pain-relieving drugs that include prescription medications like oxycodone, hydrocodone, and morphine, as well as illegal drugs like heroin. Also known as narcotics, they work by binding to special receptors in your brain and spinal cord to block pain signals. But they also affect areas that control breathing, mood, and reward—making them effective for pain but risky for your health.
Most people know opioids can cause drowsiness or constipation, but the real dangers often hide in plain sight. opioid dependence, a physical condition where your body adapts to the drug and needs it to function normally can develop in as little as a few weeks—even when taken exactly as prescribed. And when you stop, opioid withdrawal, a set of intense physical and emotional symptoms including nausea, muscle aches, anxiety, and insomnia can make quitting feel impossible without help. These aren’t just side effects—they’re warning signs that your body is changing in ways you can’t control.
Some side effects are immediate: nausea, dizziness, confusion, or slowed breathing. Others build up over time—like tolerance, where you need higher doses to get the same relief, or hormonal changes that lead to low energy, loss of libido, or even depression. Older adults are especially at risk for confusion and falls. People with breathing problems like sleep apnea or COPD can face life-threatening drops in oxygen levels. And mixing opioids with alcohol, benzodiazepines, or even some sleep aids can stop your breathing entirely. The CDC reports that over 70% of drug overdose deaths in the U.S. involve opioids, and many of those cases involve prescriptions that started out as legitimate pain relief.
What’s missing from most doctor visits is the honest conversation about alternatives. For chronic pain, physical therapy, nerve blocks, or even certain antidepressants can work better long-term with far fewer risks. For acute pain after surgery or injury, short-term opioid use may be necessary—but it should come with a clear exit plan. You shouldn’t have to choose between pain relief and your safety.
Below, you’ll find real-world guides that break down what happens when opioids interact with your body, how to spot early signs of trouble, what alternatives exist, and how to talk to your doctor without feeling judged. These aren’t theoretical articles—they’re written by people who’ve been there, and by clinicians who’ve seen the fallout. You don’t need to guess what’s normal or what’s dangerous. The answers are here.
Opioid-induced hyperalgesia is a paradoxical condition where long-term opioid use makes pain worse. Learn how it differs from tolerance, who's at risk, and what treatments actually work.
Dec, 24 2025
Opioid-induced nausea affects up to one-third of patients. Learn which antiemetics work, which don’t, and how to avoid dangerous drug interactions while keeping pain under control.
Nov, 15 2025