Hashimoto's Thyroiditis: Causes, Symptoms, and How It Affects Your Thyroid
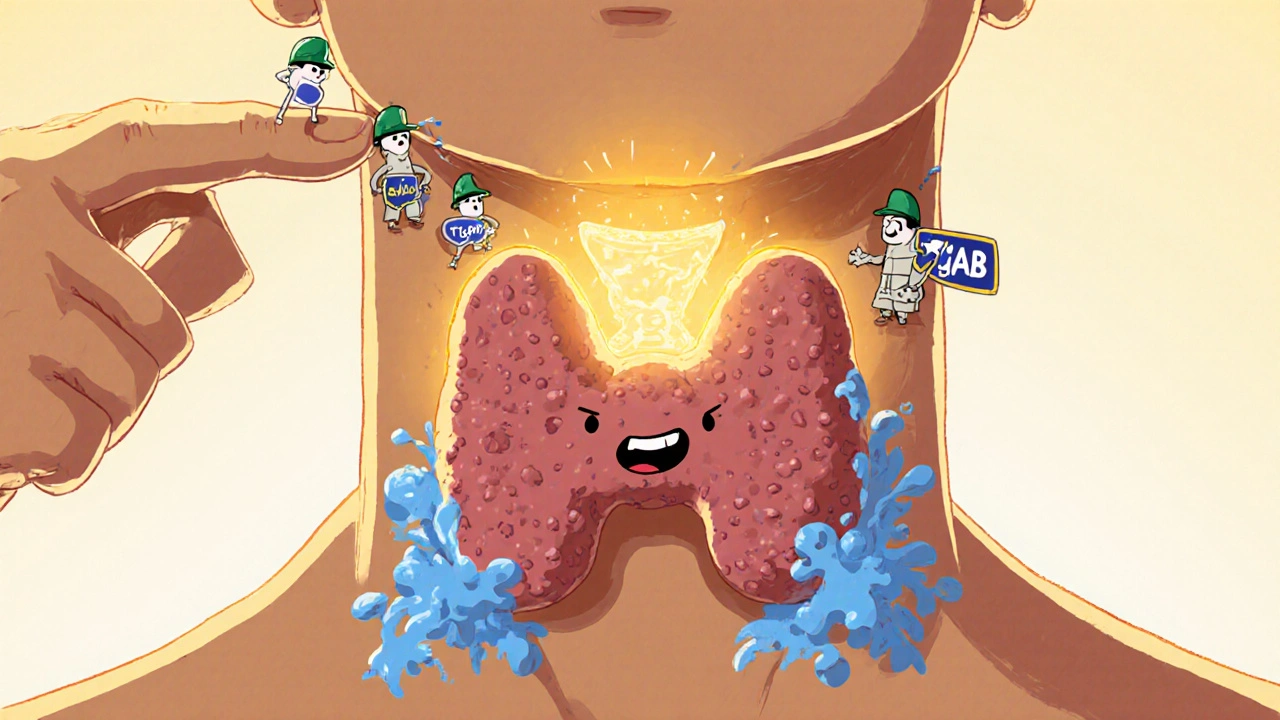
When your immune system turns against your own thyroid, you’re dealing with Hashimoto's thyroiditis, an autoimmune disorder where the body attacks thyroid tissue, leading to reduced hormone production. Also known as chronic lymphocytic thyroiditis, it’s the most common reason people end up with hypothyroidism—where your thyroid just can’t keep up with your body’s needs. Unlike sudden thyroid issues, Hashimoto’s creeps in slowly. Many people live for years with mild symptoms—fatigue, weight gain, cold hands—before someone connects the dots.
What makes Hashimoto’s different from other thyroid problems is the presence of thyroid antibodies, specific proteins your immune system produces to mistakenly target your thyroid gland. Two main ones show up in blood tests: TPOAb (thyroid peroxidase antibodies) and TGAb (thyroglobulin antibodies). High levels don’t always mean severe symptoms, but they confirm the autoimmune root. This isn’t just about your thyroid—it’s about your whole immune system going off track. Stress, genetics, and even gut health can play a role in triggering or worsening it.
Once your thyroid gets damaged, it stops making enough levothyroxine, the synthetic version of the main thyroid hormone T4 that your body needs to regulate energy, temperature, and metabolism. That’s why most people with Hashimoto’s end up on daily thyroid hormone replacement. It’s not a cure, but it’s a lifeline. You’ll need regular blood tests to fine-tune your dose—too little and you stay tired, too much and you risk heart palpitations or bone loss. It’s a balancing act, but one that millions manage successfully.
What you won’t find in most doctor’s offices is the full picture: how Hashimoto’s connects to other autoimmune conditions like celiac disease or type 1 diabetes, why some people react to gluten even without celiac, or how selenium and vitamin D might help lower antibody levels. The posts below cover these real-world details—what actually works, what doesn’t, and what to ask your doctor when your symptoms don’t match the textbook.
Hashimoto's thyroiditis is the most common cause of hypothyroidism. Learn how TSH levels are managed with levothyroxine, why symptoms persist despite 'normal' tests, and what triggers flares - backed by clinical data and patient experiences.
Nov, 16 2025