Hashimoto's Thyroiditis: Understanding Autoimmune Thyroid Disease and How to Manage TSH Levels
Hashimoto's thyroiditis is the most common cause of hypothyroidism in countries where people get enough iodine in their diet. It’s not just a slow thyroid - it’s your immune system mistakenly attacking your own thyroid gland. This isn’t something that comes on overnight. It creeps in over years, often without clear symptoms at first. By the time people feel tired, gain weight, or struggle with brain fog, the damage is already done. But here’s the good news: with the right approach to TSH management, most people can feel normal again.
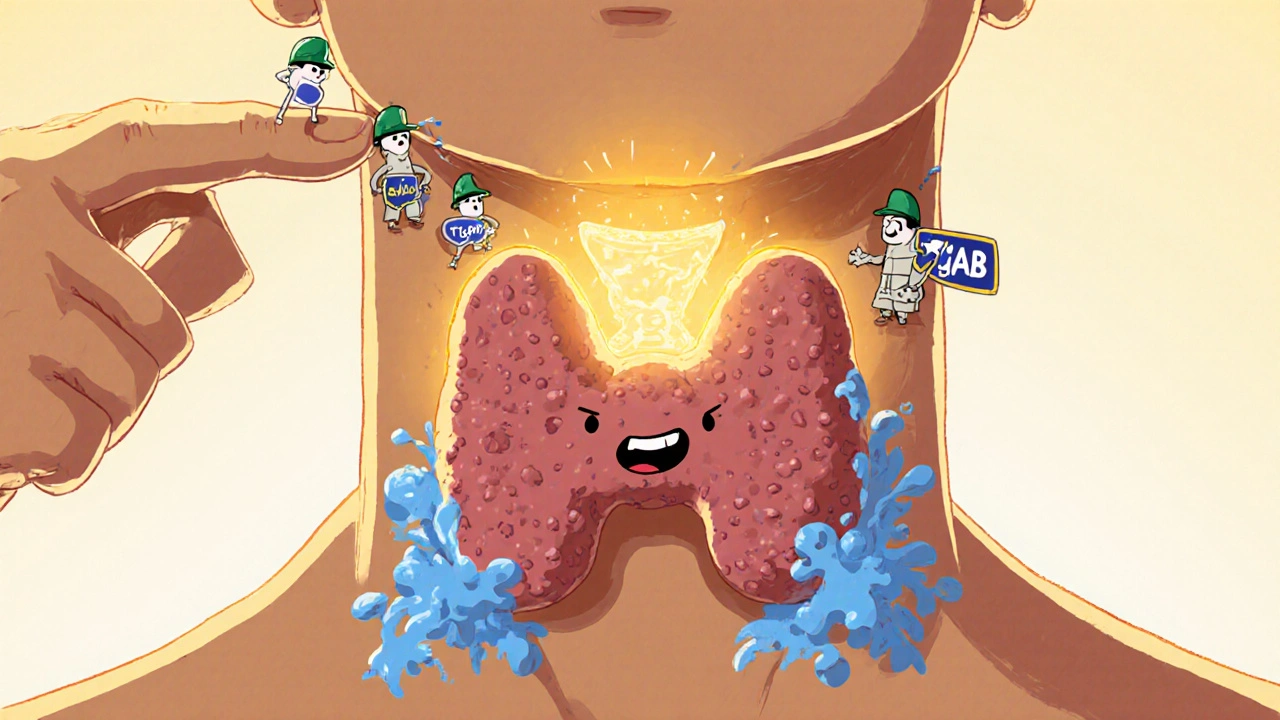
What Happens Inside Your Body With Hashimoto’s?
Your thyroid sits at the base of your neck and makes hormones that control your metabolism, energy, temperature, and heart rate. In Hashimoto’s, your immune system sends T-cells and antibodies to destroy thyroid tissue. The two main antibodies involved - thyroid peroxidase (TPOAb) and thyroglobulin (TgAb) - are found in nearly all patients. When these antibodies attack, your thyroid slowly loses its ability to produce hormones. Over time, this leads to low levels of T3 and T4, and your pituitary gland responds by pumping out more TSH - thyroid-stimulating hormone - trying to force the thyroid to work harder.
This process happens in stages. Many people start with normal thyroid function but already have high antibody levels. This is phase one. Then, TSH starts creeping up above 4.5 mIU/L while T4 stays normal - that’s subclinical hypothyroidism. Eventually, T4 drops, and you’re officially hypothyroid. Some people even go through a brief phase called hashitoxicosis, where the thyroid releases stored hormones all at once, causing temporary symptoms of hyperthyroidism: racing heart, anxiety, weight loss. It’s confusing, but it’s common. About 15-20% of people with Hashimoto’s experience this before settling into permanent hypothyroidism.
How Is Hashimoto’s Diagnosed?
There’s no single test. Diagnosis requires three things: elevated TSH, low or low-normal free T4, and positive thyroid antibodies. Ultrasound often shows a swollen, patchy thyroid with increased blood flow - a telltale sign. But here’s the catch: some people have high antibodies and normal TSH for years. Others have normal antibodies but still have Hashimoto’s. That’s why doctors don’t rely on one number. They look at the whole picture: symptoms, antibody history, TSH trends, and ultrasound findings.
One major pitfall? TSH can be falsely high because of antibodies that interfere with lab tests. If your TSH looks high but you feel fine, your doctor should check your free T4. If T4 is normal, the TSH might be misleading. This happens in 5-10% of cases. Don’t let a single number dictate your treatment.
TSH Targets: One Size Does Not Fit All
For years, doctors aimed to keep TSH between 0.5 and 5.0 mIU/L. That’s still the general range. But the truth is, optimal TSH depends on who you are.
- If you’re under 60 and feeling unwell despite a TSH of 3.5, your doctor might aim for 1.0-2.5 mIU/L.
- If you’re over 70, a TSH up to 6.0 might be safer - too low can increase heart rhythm problems.
- If you’re trying to get pregnant, aim for under 2.5 mIU/L in the first trimester. Studies show miscarriage risk jumps 2.3 times when TSH is higher.
- If you’ve had thyroid cancer, your target might be below 0.1 mIU/L - but that’s a different situation.
There’s no magic number. Your goal isn’t just to get TSH into a range - it’s to feel better. If your TSH is 2.8 and you have no energy, brain fog, or cold intolerance, you might need a slight dose increase. If your TSH is 1.2 and you’re jittery, sweating, or losing weight, you might be overmedicated.

Levothyroxine: The Standard Treatment - And Its Limits
Levothyroxine (T4) is the go-to treatment. It’s cheap, stable, and works for most people. But here’s what most patients don’t know: 10-15% of people still feel awful even when their TSH is perfectly normal. Why?
Some bodies don’t convert T4 to T3 well. T3 is the active hormone your cells use. A few patients benefit from adding T3 (liothyronine), but large studies show it doesn’t help most people. The American Association of Clinical Endocrinologists says not to use combination therapy unless you’ve tried optimizing levothyroxine for at least six months and still have symptoms.
Also, not all levothyroxine brands are the same. The FDA calls it a narrow therapeutic index drug - meaning even small differences in absorption matter. If you switch from Synthroid to a generic, your TSH might jump. Stick with one brand unless your doctor says otherwise. And never switch without retesting TSH in 6-8 weeks.
How to Take Levothyroxine Right
Getting the dose right means taking it right. Here’s what actually works:
- Take it on an empty stomach, first thing in the morning.
- Wait at least 30-60 minutes before eating or drinking anything except water.
- Avoid calcium, iron, soy, and antacids for at least 4 hours after taking it - they block absorption.
- Don’t take it with coffee. Even one cup can reduce absorption by 30%.
- Test TSH in the morning, before taking your dose. Testing after your pill gives false lows.
- Avoid biotin (hair, skin, nail supplements) for at least 24 hours before blood tests - it can make TSH look falsely low.
And yes - seasonal changes matter. TSH levels naturally rise in winter. In one study of 27,000 people, winter TSH was 1.8 mIU/L higher than summer. If you feel worse in January, it’s not just the cold - your dose might need a small winter boost.
What Triggers Flares and Instability?
Hashimoto’s isn’t just about hormones. It’s also about triggers.
Patients on Reddit and thyroid forums report the same patterns:
- Stress - High cortisol messes with T4-to-T3 conversion and increases inflammation.
- Gluten - About 32% of patients say cutting gluten improves symptoms. Why? The protein structure of gluten looks similar to thyroid tissue. Your immune system gets confused.
- Chronic infections - Epstein-Barr virus (mono), Lyme, and gut dysbiosis can keep the immune system fired up.
- Sleep deprivation - Poor sleep raises TSH and lowers T3.
- Fluctuating weight - Every 10-pound weight change may require a 12.5-25 mcg dose adjustment.
One patient survey found that 41% of people had symptom flares linked to stress, and 27% noticed worse symptoms in colder months. This isn’t coincidence - it’s biology.

Why Some People Struggle for Years
On thyroid patient forums, 68% say they needed three or more dose changes before feeling right. That’s not unusual. It takes time to find your sweet spot. Some people get misdiagnosed as depressed, anxious, or just “tired.” Others are told their TSH is “normal” and sent away - even though their free T4 is in the bottom 10% of the range.
Doctors who only check TSH miss the bigger picture. A 2018 study found that 12% of patients with persistent symptoms had normal TSH but low free T4. That’s why you need both tests. And if your doctor won’t order free T4, ask for it. You have the right to know your full hormone picture.
What’s Next? The Future of Hashimoto’s Treatment
Levothyroxine isn’t the end of the story. Researchers are now looking at ways to stop the immune attack - not just replace the hormone.
In 2022, scientists found that 25% of treatment-resistant Hashimoto’s patients have antibodies that block TSH receptors - something previously only seen in Graves’ disease. This opens the door to new targeted therapies.
Twelve clinical trials are now testing drugs that calm overactive T-cells. One targets the CTLA-4 pathway, another blocks specific inflammatory signals. If successful, these could reduce or even eliminate the need for lifelong medication by 2030.
Meanwhile, genetic testing for markers like PTPN22 and CTLA-4 is becoming more common. In the future, your TSH target might be personalized based on your DNA - not just your age or gender.
What You Can Do Today
You don’t need to wait for new drugs to feel better. Start here:
- Get your TSH and free T4 tested together - not just TSH.
- Take your medication correctly: empty stomach, no coffee, no calcium, no biotin.
- Track your symptoms: energy, mood, weight, temperature, digestion.
- Consider eliminating gluten for 3 months - many see improvement.
- Manage stress with sleep, walking, or meditation - even 20 minutes a day helps.
- Ask your doctor about seasonal dose adjustments - especially if you feel worse in winter.
- Find a doctor who listens. If you’re not improving, it’s not you - it’s the approach.
Hashimoto’s isn’t a life sentence. It’s a condition that responds well to smart, consistent management. You don’t have to live with brain fog, fatigue, or weight gain. With the right care, you can get your energy back - and keep it.
Can Hashimoto’s be cured?
No, Hashimoto’s cannot be cured - but it can be managed effectively. The immune system will continue to attack the thyroid, but with proper levothyroxine dosing and lifestyle adjustments, most people achieve full symptom relief and live normal, healthy lives. The goal isn’t to stop the autoimmune process - it’s to replace the hormones your thyroid can no longer make.
Why does my TSH keep changing even though I take my medicine every day?
Many factors affect TSH levels even with consistent dosing. Weight changes, seasonal variations (TSH rises in winter), stress, gut health, and interactions with supplements like calcium or iron can all shift your hormone balance. It’s normal to need 2-3 dose adjustments in the first year. After that, most people stabilize and only need annual checks - unless something changes.
Should I take T3 along with T4?
For most people, no. Large studies show that adding T3 doesn’t improve symptoms over levothyroxine alone in 87% of cases. The American Association of Clinical Endocrinologists recommends against routine combination therapy. Only consider it if you’ve optimized your T4 dose for at least six months and still have symptoms - and even then, only under close medical supervision.
Can gluten make Hashimoto’s worse?
Yes, for many people. Gluten shares a similar structure to thyroid tissue, which can confuse the immune system and worsen antibody activity. Studies and patient reports show that 30-40% of those with Hashimoto’s feel better after removing gluten - even if they don’t have celiac disease. A 3-month elimination trial is worth trying.
Is it safe to stop levothyroxine if I feel fine?
No. Stopping levothyroxine can lead to a dangerous drop in thyroid hormone, causing fatigue, depression, heart problems, and even myxedema coma in severe cases. Hashimoto’s destroys thyroid tissue permanently. Once it’s gone, your body can’t make enough hormone on its own. Lifelong replacement is necessary - but it’s simple and effective.
How often should I get my TSH checked?
After starting or changing your dose, test every 6-8 weeks until your levels are stable. Once stable, annual testing is usually enough - unless you gain or lose weight, become pregnant, start new medications, or feel symptoms returning. If you’re over 65 or have heart disease, your doctor may check more often to avoid overtreatment.
Can Hashimoto’s affect my mental health?
Absolutely. Low thyroid hormone affects serotonin and other brain chemicals. Depression, anxiety, brain fog, and memory problems are common symptoms - not just “in your head.” Many patients report dramatic mental clarity after optimizing their T4 dose. If you’re struggling mentally, check your TSH and free T4 - you might need a dose adjustment, not antidepressants.

Kathryn Ware
November 17, 2025 AT 22:25Okay but have y’all tried doing a 30-day gluten-free trial? I was diagnosed with Hashimoto’s in 2020 and my TSH was stuck at 6.8 for a year. Cut out gluten, added selenium, and within 8 weeks my antibodies dropped by 60%. I’m not saying it’s magic, but it’s not placebo either. My energy? Back. My brain fog? Gone. I swear by it now. 🙌
Eric Healy
November 18, 2025 AT 14:18people dont understand tsh is just a proxy its not the hormone its the signal the brain sends to the thyroid if your t4 is low and tsh is 3.5 youre still hypothyroid no matter what the guidelines say stop letting doctors play number games
Shannon Hale
November 18, 2025 AT 16:42OMG I CRIED WHEN I READ THIS. I was told for 4 years I was just 'stressed' or 'depressed' - until I found a functional doc who checked my free T4 and saw it was in the bottom 5% of the range. My TSH was 'normal' at 3.1. I was dying inside. Now I’m on a slightly higher dose and I can actually think again. Stop ignoring symptoms just because the numbers look 'fine'.
Jessica Healey
November 18, 2025 AT 16:44coffee is the devil. i switched to tea and my tsh dropped 1.2 points in 6 weeks. no joke. also biotin? dont even think about it. i got a false low tsh and my doctor almost lowered my dose. nightmare.
Levi Hobbs
November 20, 2025 AT 12:58Seasonal TSH changes are real. I had mine tested in August and it was 1.8. Came back in January after a rough winter and it was 3.9. No changes in meds, no weight gain, just winter. My doctor adjusted my dose by 12.5 mcg and I felt like a new person. Don’t ignore the seasons - your thyroid does.
Gordon Mcdonough
November 20, 2025 AT 17:47AMERICA NEEDS TO STOP GIVING OUT THYROID MEDS LIKE CANDY. EVERYONE THINKS THEY HAVE HASHIMOTO NOW. I WORKED IN A CLINIC FOR 12 YEARS AND HALF THESE PEOPLE JUST WANT TO BE SPECIAL. YOUR TSH IS 3.2 AND YOU’RE NOT DYING. TAKE A WALK. STOP WHINING.
Kiran Mandavkar
November 21, 2025 AT 06:51One must question the metaphysical underpinnings of endocrinology itself. The thyroid is not merely a gland - it is a mirror of the soul’s dissonance with modernity. TSH is not a number, it is a symptom of systemic alienation. The pharmaceutical-industrial complex profits from your suffering, not your healing. To treat Hashimoto’s with levothyroxine is to appease the machine - not restore the self. What if the cure lies not in substitution, but in radical reconnection? With nature. With silence. With the unmediated breath?
Kelsey Robertson
November 22, 2025 AT 14:40Wait - so you’re telling me the ‘normal’ TSH range is arbitrary? Shocking. Next you’ll say the sun doesn’t rise and the earth isn’t flat. I’ve had 3 doctors tell me my TSH is fine. I feel like garbage. So clearly the science is wrong. Or maybe I’m just… weak? 🤔
henry mariono
November 23, 2025 AT 01:22I appreciate the depth of this post. I’ve been managing Hashimoto’s for 7 years. I’ve tried everything - gluten-free, selenium, T3 combos. Nothing replaced the consistency of levothyroxine. I’m not looking for a miracle. Just stability. And I’m grateful this info is out there.
satya pradeep
November 24, 2025 AT 23:55bro i had tsh 8.5 and felt like a zombie. started taking t4 and now im running marathons. but yeah dont take biotin before blood test. i did that once and got a false 0.9. my doc thought i was overmedicated. i almost stopped my meds. dumb. check your labs before you take your pill. also sleep matters. no more 3am scrolling.
Holli Yancey
November 26, 2025 AT 13:51I’m not sure why people get so heated about this. It’s just a hormone imbalance. You take a pill, you feel better. If you don’t feel better, maybe it’s not the thyroid. Maybe it’s your diet, your sleep, your mindset. I’ve seen too many people cling to Hashimoto’s as an identity. It’s a medical condition, not a lifestyle brand.
Joseph Peel
November 26, 2025 AT 16:52In Japan, we treat subclinical hypothyroidism differently. We don’t rush to levothyroxine unless TSH is above 7.0 and symptoms are clear. We focus on diet - seaweed, fermented foods, stress reduction. Maybe we’re too conservative. But maybe we’re not rushing to medication before addressing root causes.
Elia DOnald Maluleke
November 26, 2025 AT 19:09Let us contemplate the nature of the immune system’s betrayal. Is Hashimoto’s not a metaphor for modern life? We consume toxins, we sleep poorly, we are disconnected from community - and our bodies, in their infinite wisdom, turn against themselves. The pill is a bandage. The cure is a revolution in how we live. But who among us dares to change?
Joseph Townsend
November 27, 2025 AT 07:30I went from crying in the shower every morning to running 10Ks in 6 months. This isn’t just ‘thyroid stuff’ - it’s a goddamn life-or-death situation. I was told I was ‘anxious’ and given Xanax. I was dying. Now I’m alive. Don’t let anyone tell you it’s ‘all in your head.’
Sridhar Suvarna
November 28, 2025 AT 17:58