Dopamine Agonists – What They Are and Why They Matter
When working with dopamine agonists, medications that mimic dopamine activity in the brain. Also known as dopaminergic agents, they bind to dopamine receptors to boost signaling where it’s low.
Key Conditions Treated by Dopamine Agonists
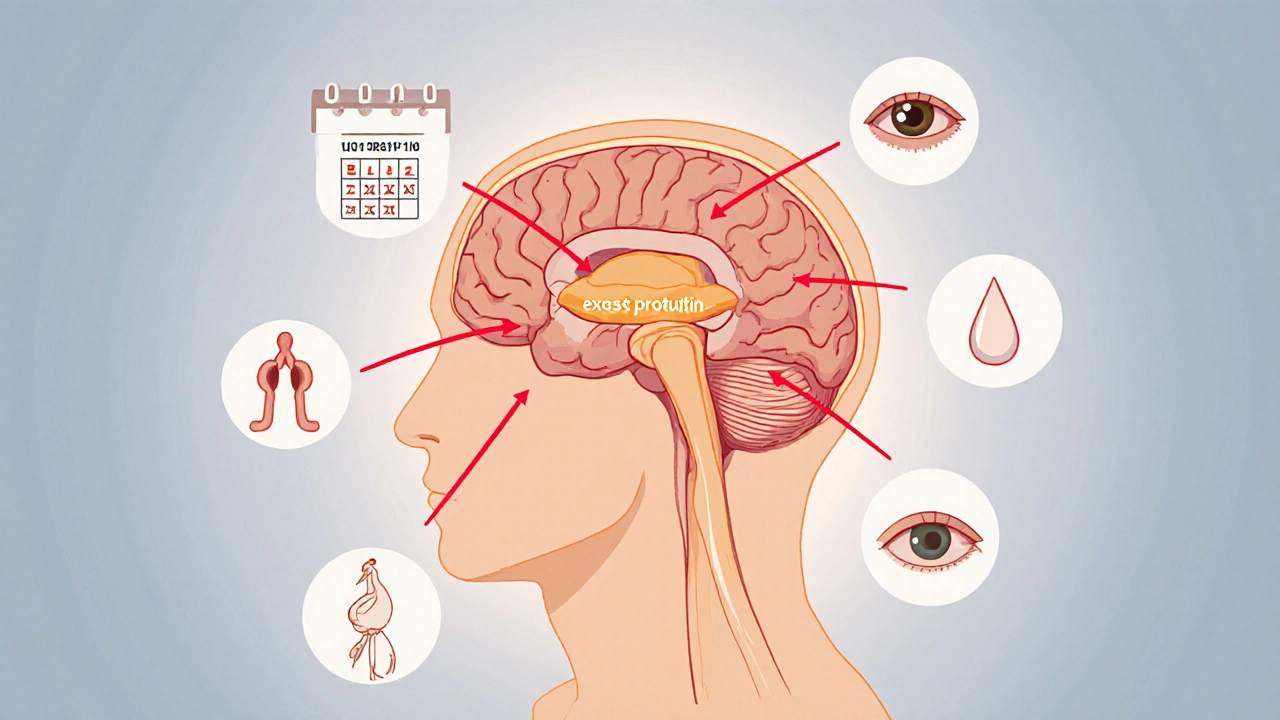
One of the main reasons doctors prescribe them is for Parkinson's disease, a neurodegenerative disorder characterized by tremor, rigidity, and slowed movement. By activating D2 receptors, these drugs help restore motor control and reduce "off" periods. Prolactinoma, a benign pituitary tumor that overproduces prolactin is another target; dopamine agonists suppress excess prolactin, shrinking the tumor and normalizing hormone levels. People with restless leg syndrome, an urge to move the legs, especially at night also find relief because the drugs improve dopaminergic signaling that regulates limb movement.
Beyond these therapeutic wins, there are trade‑offs. A common semantic triple is: "Dopamine agonists can trigger impulse control disorders," meaning patients may develop compulsive gambling, shopping, or eating. Another link: "Long‑term use may lead to morning nausea," which often eases with dose adjustments. They also interact with antipsychotics that block dopamine, so clinicians must balance benefits against potential worsening of psychosis. Understanding how these agents fit into broader treatment plans—whether as monotherapy or alongside levodopa—helps you weigh efficacy against side‑effects.
Below you’ll see a curated list of articles that break down each drug class, compare popular options, and give practical tips for monitoring safety. Whether you’re new to the topic or looking for deeper insight, the collection offers clear guidance on choosing and managing dopamine agonist therapy.
Explore medication and surgery options for hyperprolactinaemia, learn how dopamine agonists work, when surgery is needed, and how to monitor treatment effectively.
Oct, 12 2025