Cabergoline Dosage: What You Need to Know
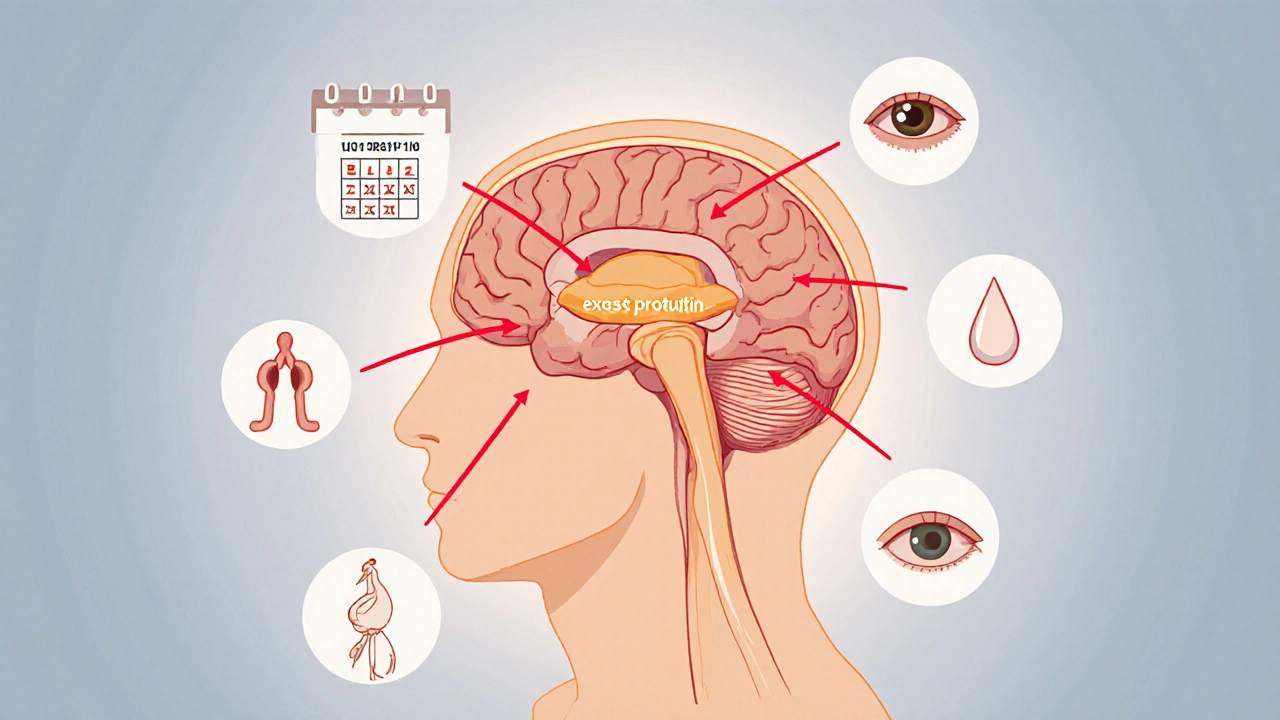
When talking about cabergoline dosage, the amount of the dopamine agonist prescribed to lower excess prolactin or manage Parkinson's symptoms. Also known as CAB, it works by stimulating dopamine receptors in the brain, which in turn suppresses prolactin release from the pituitary gland. Prolactinoma, a benign pituitary tumor that overproduces prolactin often requires a careful titration plan, while dopamine agonist, a class of drugs that mimic dopamine activity like cabergoline is the first‑line therapy. In Parkinson’s disease, the same drug is used at different intervals, showing that cabergoline dosage encompasses both endocrine and neurological contexts. A typical semantic triple here is: Cabergoline dosage requires regular prolactin level checks; Prolactinoma influences dose titration; Dopamine agonist affects Parkinson’s symptom control. Understanding these links helps you set realistic expectations before starting treatment.
Key Factors That Shape Your Dose
First, the initial dose depends on the condition. For prolactinoma, doctors often start with 0.25 mg twice a week and increase by 0.25 mg increments every few weeks until prolactin normalizes. In Parkinson’s, the starting point can be 0.5 mg once daily, with adjustments based on motor function and side‑effect tolerance. Side effects, nausea, low blood pressure, and rare heart valve issues are dose‑dependent, so regular monitoring is a must. Blood pressure checks, echocardiograms, and prolactin labs create a feedback loop: the test results inform whether to maintain, increase, or reduce the dose. Age, kidney function, and other medications also play a role; for example, patients on antihypertensives may need a slower ramp‑up to avoid dizziness. Remember that cabergoline has a long half‑life, so missed doses should be taken as soon as remembered, but never double up – doing so can push the dose beyond safe limits.
Finally, real‑world experience shows that most patients find a stable dose within 3‑6 months. Once the target prolactin level is hit, many stay on the same regimen for years, occasionally tapering if the tumor shrinks or symptoms improve. For Parkinson’s, dose tweaks are more frequent, reflecting the progressive nature of the disease. The common thread is a partnership between you and your healthcare provider: clear communication, adherence to lab schedules, and awareness of how each adjustment may impact your daily life. Below you’ll find a curated collection of articles that dive deeper into specific dosing strategies, side‑effect management, and comparison with other dopamine agonists. Use them as a roadmap to keep your treatment on track.
Explore medication and surgery options for hyperprolactinaemia, learn how dopamine agonists work, when surgery is needed, and how to monitor treatment effectively.
Oct, 12 2025