Weight Loss Medications: GLP-1 Agonists vs. Older Drugs
When it comes to losing weight, not all medications are created equal. Over the past five years, a new wave of drugs has taken center stage in weight management - GLP-1 agonists like Wegovy, Zepbound, and Saxenda. These aren’t just updated versions of old pills. They work differently, work better, and cost a lot more. Meanwhile, older options like orlistat, Qsymia, and phentermine are still around, but they’re playing catch-up. So which one actually works for you? It’s not just about the scale. It’s about side effects, cost, how you take it, and whether you can stick with it long-term.
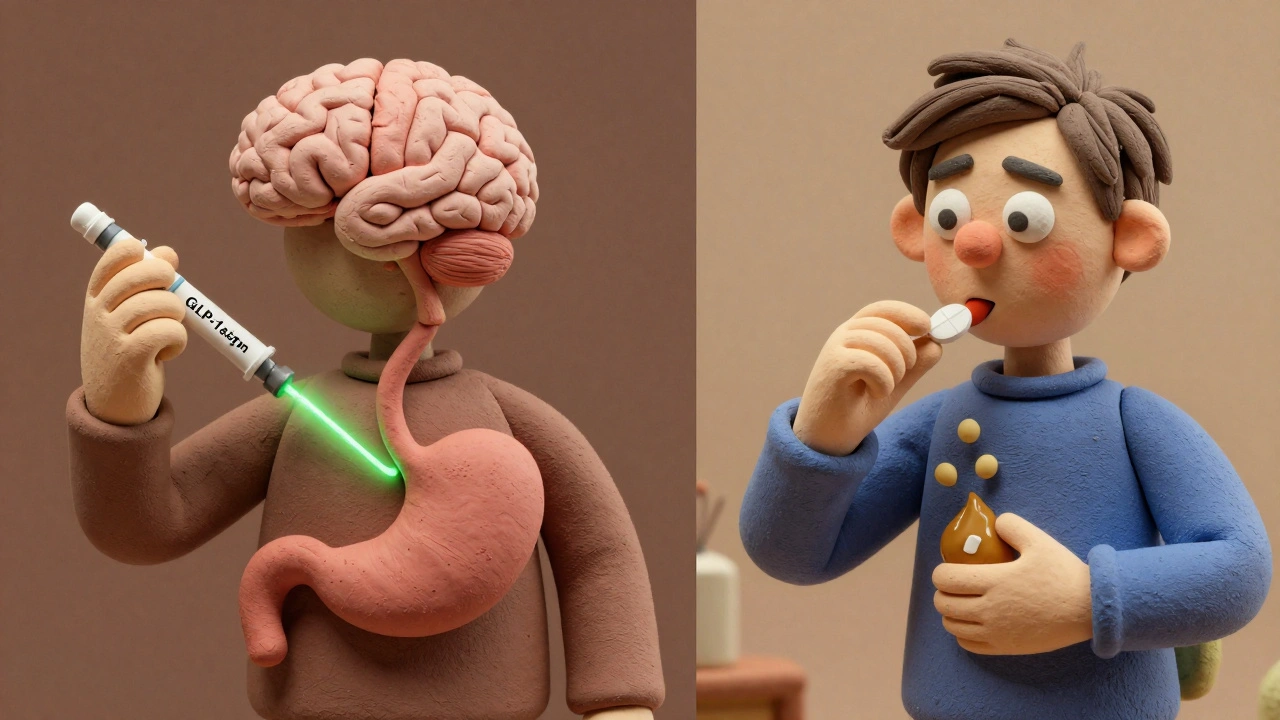
How GLP-1 Agonists Actually Work
GLP-1 agonists mimic a natural hormone your body makes after eating. That hormone - glucagon-like peptide-1 - tells your brain you’re full and slows down how fast your stomach empties. It also helps your pancreas release insulin when blood sugar rises. That’s why these drugs were first made for type 2 diabetes. But doctors noticed something unexpected: patients lost a lot of weight. Really a lot.
Wegovy (semaglutide) and Zepbound (tirzepatide) are the heavy hitters. In clinical trials, people on Wegovy lost an average of 14.7% of their body weight in under a year. Zepbound, which hits two hormone receptors instead of one, pushed that number to over 20%. Compare that to older drugs: orlistat (Alli) blocks fat absorption, so you pass undigested grease in your stool - not exactly pleasant. People typically lose 5-10% with it. Phentermine-topiramate (Qsymia) suppresses appetite but can cause dry mouth, tingling, and mood changes. Naltrexone-bupropion (Contrave) targets brain reward pathways, but most users still only shed around 8%.
The difference isn’t small. It’s dramatic. One head-to-head study showed Wegovy users lost 16% of their weight versus 6% on Saxenda - and Saxenda is itself a GLP-1 drug. That’s not a minor upgrade. It’s a revolution.
Older Weight Loss Drugs: What’s Still Working
Just because newer drugs exist doesn’t mean the old ones are useless. Orlistat (Xenical, Alli) has been on the market since the late 1990s. It’s available over the counter in lower doses. It’s cheap - often under $50 a month - and doesn’t affect your brain. But it comes with a trade-off: oily spotting, frequent bowel movements, and the need to strictly limit fat intake. If you love fried food, this isn’t for you.
Phentermine is a stimulant, similar to amphetamines. It’s been used since the 1950s. It works fast - many people see weight loss in the first few weeks. But it’s only approved for short-term use (12 weeks or less) because of risks like increased heart rate and high blood pressure. It’s often paired with topiramate (Qsymia) to extend its effects. That combo can help people lose up to 10% of their body weight, but side effects like brain fog, memory issues, and insomnia are common.
Contrave combines naltrexone (used for addiction) and bupropion (an antidepressant). It’s meant to reduce cravings and make food less rewarding. It’s not a magic bullet. Most users lose around 5-8% and need to take it daily for months before seeing results. It’s also not safe for people with seizure disorders or uncontrolled high blood pressure.
These older drugs aren’t going away. They’re still prescribed - especially when insurance won’t cover the newer options. But their effectiveness is modest, and many patients get frustrated by slow progress.
Cost and Insurance: The Real Barrier
Here’s where things get messy. GLP-1 agonists cost between $1,000 and $1,400 a month without insurance. That’s $12,000 to $16,800 a year. Even with manufacturer coupons, you’re still paying hundreds a month. And those coupons often cap at $500-$1,000 in savings per year.
Insurance coverage is a nightmare. Only 28% of commercial insurance plans cover GLP-1 drugs for weight loss without strict rules. Many require a BMI over 35 with a related condition like diabetes or high blood pressure. Some won’t cover them at all unless you’ve tried and failed diet and exercise first. And even then, prior authorizations get denied 45% of the time, according to patient surveys.
Meanwhile, older drugs are dirt cheap. Phentermine can cost as little as $10 a month. Orlistat runs $30-$50. Qsymia and Contrave are pricier - around $100-$150 - but still a fraction of the cost of Wegovy. For people without good insurance, the choice isn’t about which drug is better. It’s about which one they can afford.

Side Effects: Not Just Nausea
Everyone talks about nausea. And yes, it’s common. Up to 50% of people on GLP-1 drugs feel sick, especially when starting or increasing the dose. But that’s just the start. Vomiting, diarrhea, constipation, and bloating are frequent. Some users report gastroparesis - a condition where the stomach stops emptying properly - leading to severe pain and malnutrition.
And it’s not just GI issues. A 2024 study found that 70% of people stop taking GLP-1 drugs within a year. Why? Cost, side effects, or because the weight loss stalled. Real-world results are lower than clinical trial numbers. One NYU Langone study found patients lost only 4.7% after six months - far below the 15%+ seen in trials.
Older drugs have side effects too. Phentermine can cause anxiety, insomnia, and palpitations. Orlistat leads to embarrassing bathroom accidents. Qsymia carries a risk of birth defects - women must use birth control. Contrave can raise blood pressure and increase seizure risk.
But here’s the catch: GLP-1 side effects are often temporary. They usually improve after the first few weeks as your body adjusts. Many patients who stick through the initial nausea end up with life-changing results.
Administration: Injections vs. Pills
Wegovy and Zepbound come as weekly injections. Saxenda is daily. You have to learn how to give yourself a shot. For some, that’s easy. For others, it’s a dealbreaker. Fear of needles, discomfort with self-injection, or simply forgetting the routine can derail progress.
Oral semaglutide (Rybelsus) exists, but it’s approved only for diabetes, not weight loss - and it’s not as effective as the injectable. All the older drugs are pills. You swallow them once a day. No needles. No training. No fear. That’s a big advantage for people who just want something simple.
But let’s be honest: if you’re serious about losing 20% of your body weight, you’re probably willing to deal with a needle. The bigger issue is consistency. Missing one injection can throw off your progress. Missing a pill? Less likely to matter.
What Happens When You Stop?
This is the question no one wants to ask - but you need to know. If you stop taking a GLP-1 agonist, you’ll likely regain the weight. Studies show 50-100% of lost weight comes back within a year of stopping. That’s not a failure. It’s biology. These drugs don’t fix your metabolism. They temporarily suppress appetite and slow digestion. Once you stop, your body reverts to its old patterns.
Older drugs have the same problem. Stop phentermine? Weight returns. Stop orlistat? You gain back what you lost. The difference is, GLP-1 drugs create such dramatic weight loss that the rebound feels more shocking. Losing 50 pounds and gaining back 40 is harder to accept than losing 10 and gaining back 8.
That’s why experts now say these drugs aren’t meant to be taken forever. They’re meant to jumpstart change - to help you build habits, improve your relationship with food, and maybe even prepare you for surgery if needed. They’re tools, not cures.

Who Should Use Which?
Let’s cut through the noise. Who benefits most from each?
Choose GLP-1 agonists if:
- You need to lose 15% or more of your body weight
- You have type 2 diabetes or prediabetes
- You can afford the cost or have good insurance coverage
- You’re okay with weekly injections
- You’re willing to manage nausea during the first few months
Choose older drugs if:
- You need to lose 5-10% and want something affordable
- You can’t get insurance to cover GLP-1 drugs
- You’re needle-averse
- You prefer daily pills over injections
- You have a BMI under 35 and no major health conditions
There’s no one-size-fits-all. A 45-year-old woman with a BMI of 42 and type 2 diabetes might do great on Zepbound. A 30-year-old man with a BMI of 30 and no medical issues might do fine on orlistat - if he’s willing to cut out cheeseburgers.
The Future: What’s Coming Next
GLP-1 drugs aren’t the end of the road. Newer versions are already in the pipeline. Retatrutide - a triple agonist targeting GLP-1, GIP, and glucagon - showed 24.2% weight loss in early trials. MariTide, a monoclonal antibody from Amgen, is now in Phase 3 testing and could offer similar results without injections.
Patents for semaglutide expire around 2030. That means generic versions could drop prices dramatically. Until then, manufacturers are racing to lock in market share. Novo Nordisk and Eli Lilly are spending billions on marketing, patient support programs, and even insurance advocacy.
Meanwhile, bariatric surgery remains the gold standard for long-term weight loss. A 2024 study showed surgery patients lost 24% of their body weight after two years - nearly double what GLP-1 users achieved in the same time. Experts say: if you’re not getting results with medication, or you can’t afford it, surgery is still the most effective option.
Final Thoughts: It’s Not Just About the Drug
Weight loss meds - whether new or old - aren’t magic. They’re tools. They work best when paired with real lifestyle changes: better food, movement, sleep, and stress management. No pill will fix a diet full of ultra-processed foods. No injection will undo years of emotional eating.
The biggest mistake people make is thinking the drug is the solution. It’s not. It’s the catalyst. The real work - learning to eat differently, moving your body regularly, managing stress - happens whether you’re on Wegovy or orlistat.
If you’re considering one of these drugs, talk to your doctor. Ask about your goals. Ask about cost. Ask about side effects. Ask what happens if you stop. And most importantly - ask yourself: are you ready to change your life, not just your weight?
Are GLP-1 agonists better than older weight loss drugs?
Yes, in terms of effectiveness. GLP-1 agonists like Wegovy and Zepbound typically help people lose 15-20% of their body weight, while older drugs like orlistat or phentermine usually lead to 5-10% loss. GLP-1s also offer benefits for blood sugar and heart health. But they’re more expensive, require injections, and have stronger side effects. So "better" depends on your goals, budget, and tolerance.
Can I take GLP-1 agonists without insurance?
You can, but it’s very expensive - around $1,000-$1,400 a month. Some manufacturers offer coupons that reduce costs by up to $1,000 per year, but you’ll still pay hundreds monthly. Patient assistance programs exist, but they require income verification and have limits. Most people without insurance find older, cheaper options like orlistat or phentermine more practical.
Do GLP-1 agonists cause long-term side effects?
The most common side effects - nausea, vomiting, diarrhea - usually improve after the first few weeks. Long-term risks are still being studied, but current data shows no major organ damage. However, sudden weight regain after stopping is common. Some users report gallbladder problems or pancreatitis, but these are rare. Always discuss your personal risk factors with your doctor.
How long should I stay on a weight loss medication?
There’s no fixed timeline. Many people stay on GLP-1 drugs for years, especially if they have diabetes or obesity-related health issues. But experts recommend using them as a bridge to lifestyle change. If you stop, weight often returns. The goal is to use the medication to create space for lasting habits - not to rely on it forever.
Can I switch from an older drug to a GLP-1 agonist?
Yes, but you should do it under medical supervision. Switching requires stopping the old drug first, then starting the GLP-1 at a low dose to avoid side effects. Your doctor will help you time the transition and monitor for interactions, especially if you’re on other medications for diabetes, blood pressure, or depression.
Is bariatric surgery better than GLP-1 drugs?
For people with severe obesity (BMI ≥40), surgery leads to more weight loss - around 24% after two years - and better long-term results than medication. It’s also more durable. But it’s invasive, expensive, and carries surgical risks. GLP-1 drugs are non-surgical and reversible. Many doctors now recommend trying medication first, then considering surgery if results aren’t enough.

Raja Herbal
December 8, 2025 AT 08:29Rich Paul
December 9, 2025 AT 08:16Delaine Kiara
December 9, 2025 AT 09:38Ruth Witte
December 11, 2025 AT 07:22Katherine Rodgers
December 13, 2025 AT 01:07Lauren Dare
December 13, 2025 AT 16:33Gilbert Lacasandile
December 15, 2025 AT 11:35Kathy Haverly
December 17, 2025 AT 05:18Graham Abbas
December 19, 2025 AT 02:33Steve Sullivan
December 19, 2025 AT 13:33