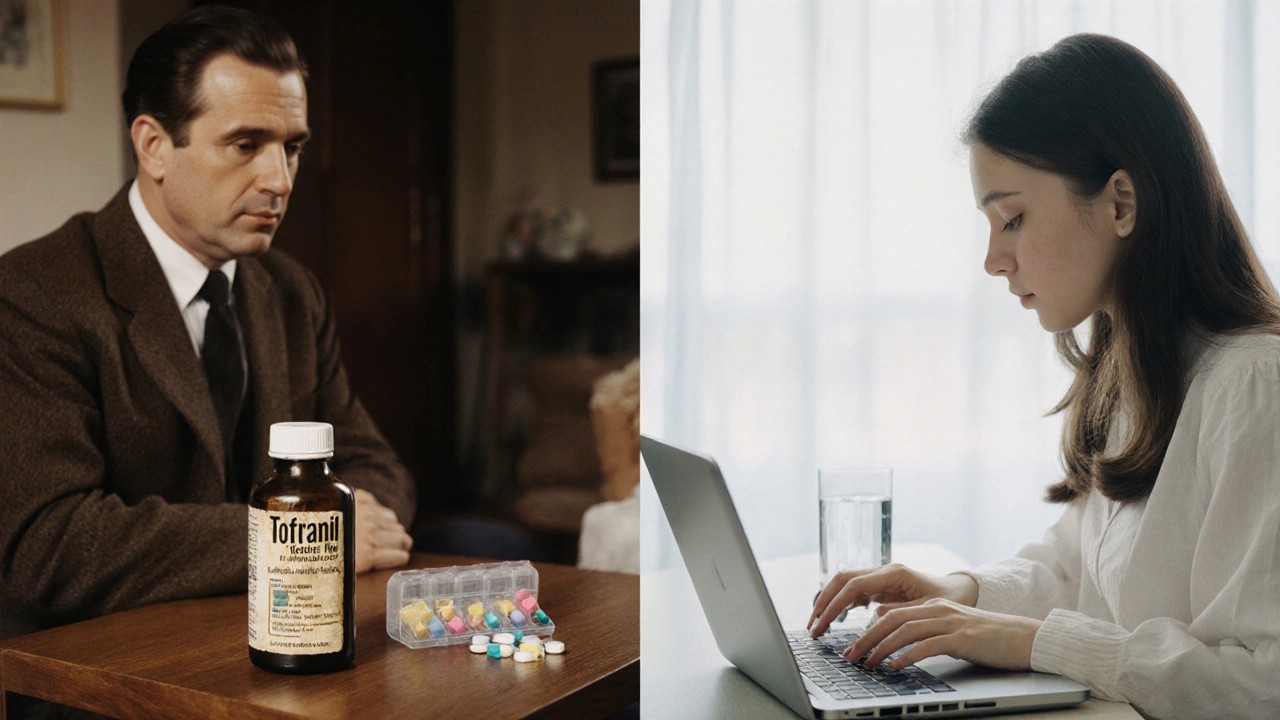
Tofranil (Imipramine) vs. Alternatives: A Comparative Guide

Antidepressant Comparison Tool
Choose Your Symptoms and Preferences
Select your primary concerns and preferences to see how Tofranil compares with newer antidepressants:
When treating major depressive disorder, Tofranil is a tricyclic antidepressant (TCA) whose generic name is imipramine. It works by increasing the levels of norepinephrine and serotonin in the brain, helping to lift mood and reduce anxiety. If you’ve been prescribed this drug or are considering it, you probably wonder how it stacks up against newer options. Below you’ll find a side‑by‑side look that cuts through the jargon and tells you what really matters for everyday decisions.
TL;DR
- Tofranil (imipramine) is a TCA; newer drugs like SSRIs and SNRIs usually have milder side‑effects.
- It shines for patients who need help with insomnia, appetite loss, or chronic pain.
- Typical starting dose is 75mg/day, titrated up to 300mg; alternatives start lower (20‑50mg for SSRIs).
- Drug interactions are plentiful - watch out for MAO inhibitors, antihistamines, and certain heart meds.
- Cost‑wise, Tofranil is cheap, but you may spend more on monitoring and managing side‑effects.
What Is Tofranil (Imipramine)?
Imipramine was first approved in the late 1950s, making it one of the earliest antidepressants on the market. It belongs to the tricyclic class, a group named for their three-ring chemical structure. While newer drugs target serotonin more selectively, Tofranil blocks the reuptake of both serotonin and norepinephrine, giving it a broader neurotransmitter impact.
Beyond depression, clinicians also use it for panic disorder, nocturnal enuresis in children, and certain types of chronic neuropathic pain. The drug’s versatility comes from its ability to modulate several brain pathways at once.
How Does It Work?
The central action is “reuptake inhibition.” By preventing neurons from pulling serotonin and norepinephrine back into the cell, the drug leaves more of these chemicals hanging around in the synaptic cleft, which improves mood and reduces anxiety. It also has mild anticholinergic effects, meaning it can dry the mouth and cause constipation - side‑effects that older patients often notice.
Alternatives at a Glance
Modern psychiatry leans heavily on selective serotonin reuptake inhibitors (SSRIs) and serotonin‑norepinephrine reuptake inhibitors (SNRIs). Below are the most commonly prescribed cousins of Tofranil.
Fluoxetine is an SSRI best known as Prozac, used for depression, OCD, and bulimia.
Sertraline is another SSRI, marketed as Zoloft, popular for depression and PTSD.
Venlafaxine is an SNRI that treats major depressive disorder and generalized anxiety.
Bupropion is an atypical antidepressant that also helps with smoking cessation.
Mirtazapine is an atypical agent that can boost appetite and improve sleep.
Side‑Effect Profiles: Tofranil vs. the New Kids
Tofranil carries a higher burden of anticholinergic side‑effects: dry mouth, blurred vision, urinary retention, and constipation. Cardiac conduction issues (QT prolongation) also warrant ECG monitoring for older adults or those with heart disease. Weight gain is less common than with some atypicals, but insomnia can be a problem because the drug is mildly stimulating at lower doses.
SSRIs such as fluoxetine and sertraline tend to cause gastrointestinal upset, sexual dysfunction, and occasional insomnia, but they lack the serious cardiac concerns of TCAs. SNRIs like venlafaxine can raise blood pressure at higher doses, while bupropion’s stimulant‑like action may trigger anxiety in sensitive people. Mirtazapine often improves sleep and appetite, but it can cause significant weight gain and sedation.
When Might Tofranil Be the Better Choice?
- Insomnia or early‑morning awakening: Low‑dose Tofranil can be mildly activating, helping patients get out of bed.
- Chronic pain: Its norepinephrine boost has analgesic benefits that SSRIs lack.
- Treatment‑resistant depression: Some patients who don’t respond to SSRIs find relief with a TCA.
- Cost sensitivity: Generic imipramine is often cheaper than brand‑name SSRIs or SNRIs.
Conversely, if you have a history of heart rhythm problems, are on multiple medications that interact via the cytochrome P450 system, or are elderly, newer agents with cleaner safety profiles may be safer.
Practical Considerations
Dosage and Titration
Typical adult initiation starts at 75mg once daily, usually taken at bedtime because of its sedating effect. Physicians often split the dose (e.g., 25mg in the morning, 50mg at night) to balance activation and sleep. The maximum recommended dose is 300mg per day, but many patients find adequate relief at 150-200mg.
Drug Interactions
Tofranil is metabolized by CYP2D6 and CYP3A4. Combining it with MAO inhibitors, SSRIs, or other serotonergic agents can trigger serotonin syndrome. Antihistamines, anticholinergics, and certain antiarrhythmics amplify cardiac risks. Always review your full medication list with your prescriber.
Tapering and Discontinuation
Because TCAs have a relatively long half‑life, a gradual taper over 2-4 weeks reduces withdrawal symptoms like dizziness, flu‑like malaise, and mood swings. Never stop abruptly.
Cost and Accessibility
In Australia, generic imipramine costs roughly AUD5-10 for a month’s supply, while brand‑name SSRIs may run AUD30-50 unless covered by PBS. However, the hidden cost of extra appointments for ECGs or blood work can narrow the price gap.
Decision Checklist
- Do you have a history of heart rhythm issues? Yes → consider SSRIs/SNRIs.
- Is insomnia a big problem? Yes → low‑dose Tofranil or mirtazapine may help.
- Are you taking lots of other meds that affect CYP enzymes? Yes → watch for interactions.
- Is cost a primary concern? Yes → imipramine is inexpensive.
- Have you tried an SSRI without success? Yes → a TCA trial could be worthwhile.
Quick Reference Table
| Drug | Class | Typical Starting Dose | Common Side Effects | Notable Advantages |
|---|---|---|---|---|
| Tofranil (Imipramine) | Tricyclic Antidepressant | 75mg nightly | Dry mouth, constipation, cardiac QT prolongation | Effective for pain, insomnia; low cost |
| Fluoxetine | SSRI | 20mg daily | GI upset, sexual dysfunction, insomnia | Long half‑life, good for adherence |
| Sertraline | SSRI | 50mg daily | Diarrhea, sexual dysfunction, anxiety | Well‑tolerated, broad FDA approvals |
| Venlafaxine | SNRI | 75mg daily | Increased blood pressure, nausea | Dual serotonin‑norepinephrine action |
| Bupropion | Atypical Antidepressant | 150mg daily | Insomnia, dry mouth, seizure risk at high doses | Helps with smoking cessation, minimal sexual side‑effects |
| Mirtazapine | Atypical Antidepressant | 15mg at bedtime | Weight gain, sedation | Improves sleep, appetite; useful for anxious depression |

Frequently Asked Questions
Is Tofranil safe for long‑term use?
Yes, many patients stay on imipramine for years, but they need regular cardiac monitoring and periodic reviews for side‑effects. The key is individualized risk assessment.
How quickly does Tofranil start working?
Therapeutic effects usually appear after 2-4 weeks, similar to most antidepressants. Early improvements in sleep or appetite may be noticed sooner.
Can I take Tofranil with an SSRI?
Co‑administration is generally discouraged because of the risk of serotonin syndrome and additive cardiac effects. If a combination is absolutely needed, it must be done under close medical supervision.
What should I do if I miss a dose?
Take the missed tablet as soon as you remember unless it’s close to the next scheduled dose. In that case, skip the missed one and continue with the regular schedule - don’t double‑dose.
Is there a generic version of Tofranil?
Yes, imipramine is available as a generic tablet in most pharmacies, which makes it a budget‑friendly option compared with many brand‑name newer agents.

Richa Ajrekar
September 28, 2025 AT 17:40Despite the detailed guide, the grammar mistakes are glaring and deserve a rewrite.
Benjamin Hamel
October 1, 2025 AT 01:13The guide paints Tofranil as a relic, yet it conveniently glosses over the fact that many so‑called “newer” agents have their own hidden pitfalls.
First, the cost argument is oversimplified; while imipramine is cheap per tablet, the cumulative expense of cardiac monitoring can eclipse the price of a brand‑name SSRI.
Second, labeling TCAs as uniformly more sedating ignores dose‑dependent activation that, at low levels, actually improves sleep architecture.
Third, the article’s claim that SSRIs have milder side‑effects fails to mention the pervasive sexual dysfunction that drives many patients off treatment.
Moreover, the emphasis on QT prolongation neglects the fact that many SSRIs, such as citalopram, also carry a black‑box warning for cardiac arrhythmias.
In addition, the drug‑interaction section understates the role of CYP2D6 polymorphisms that can turn a standard dose of imipramine into a toxic regimen.
The recommendation to avoid TCAs in severe heart disease is sound, but the blanket statement that they are unsafe for anyone with “mild issues” is unsupported by recent meta‑analyses.
Similarly, the brief nod to chronic pain ignores robust evidence that norepinephrine reuptake inhibition can reduce neuropathic pain more effectively than duloxetine in some cohorts.
While the table lists dry mouth and constipation, it forgets the anticholinergic burden that can precipitate delirium in elderly patients.
Conversely, the guide praises mirtazapine’s appetite‑boosting effect but does not address the profound weight gain that can be detrimental in metabolic syndrome.
From a pharmacoeconomic standpoint, the generic status of imipramine does reduce pharmacy out‑of‑pocket costs, but the hidden costs of lab work and specialist visits must be factored in.
The discussion on tapering is adequate, however, a gradual 2‑week taper may still be too abrupt for patients on high doses.
Finally, the guide could benefit from a more nuanced decision tree that incorporates patient preference for sleep versus weight changes.
In short, the comparison is a solid starting point but requires a deeper dive into the real‑world complexities of each medication class.
Christian James Wood
October 2, 2025 AT 05:00While the previous analysis attempts to be exhaustive, it sidesteps the core patient experience-most people on Tofranil report a relentless dry mouth that no amount of sugar‑free gum alleviates. The emotional toll of that constant discomfort often leads to non‑adherence long before any cardiac monitoring becomes relevant. Moreover, the claim that low‑dose activation helps insomnia is a double‑edged sword; many patients end up oscillating between sleeplessness and agitation. The guide also glosses over the fact that serotonin syndrome, though rare, can be precipitated by even modest CYP inhibitors. From a clinical standpoint, the recommendation to split doses is sound, yet it fails to address the practical challenges of timing for shift workers. The emphasis on cost ignores the broader socioeconomic impact of missed work days due to side‑effects. In practice, the “one‑size‑fits‑all” tone of the article feels disconnected from the nuanced decision‑making required in real clinics. Ultimately, the guide would serve patients better by foregrounding tolerability over theoretical pharmacology.
Roger Cole
October 3, 2025 AT 08:46I appreciate the thorough breakdown; the side‑effect tables are especially handy.
It’s useful to see the cost comparison laid out so clearly.
Frank Pennetti
October 4, 2025 AT 12:33The presented data, albeit superficially curated, suffers from an absence of pharmacokinetic granularity, particularly regarding imipramine’s biotransformation via CYP2D6 polymorphic pathways, which can precipitate plasma concentrations exceeding therapeutic windows by up to 300%. Moreover, the analysis neglects the impact of alpha‑1 adrenergic antagonism on orthostatic hypotension-a non‑trivial consideration in polypharmacy contexts. The cost‑effectiveness model appears to employ a static discount rate, failing to incorporate dynamic health‑economic variables such as indirect costs from work absenteeism. In addition, the cardiotoxicity risk stratification lacks a quantitative risk ratio, rendering the recommendation to “avoid TCAs in severe heart disease” qualitatively vague. A more rigorous meta‑analytic synthesis would bolster the claim hierarchy and satisfy evidence‑based scrutiny.
Adam Baxter
October 5, 2025 AT 16:20Great guide! Super helpful for anyone weighing options.
Jackie Berry
October 6, 2025 AT 20:06Thanks for the boost! I think the guide does a solid job of breaking down the pros and cons, especially for folks who are new to antidepressant therapy. It’s also nice to see the practical tips about dosing and tapering woven into the narrative. Overall, it feels like a friendly hand‑holding session rather than a dry textbook.
Mikayla May
October 7, 2025 AT 23:53The comparison table is a quick win-I bookmarked it for future reference. It’s helpful that the article mentions both efficacy and side‑effects without leaning too heavily on marketing language. The note about drug interactions with CYP enzymes is spot‑on for clinicians who manage complex regimens. I’ll definitely share this with a colleague who’s considering switching a patient from an SSRI to a TCA.
Jimmy the Exploder
October 9, 2025 AT 03:40not sure why they bother with all the tables its just a bunch of words that dont add much
Robert Jackson
October 10, 2025 AT 07:26Upon meticulous examination of the presented material, it becomes evident that the authors have engaged in a superficial synthesis of the extant literature, thereby compromising the scholarly integrity of the comparative analysis. The omission of randomized controlled trial data pertaining to imipramine’s efficacy in treatment‑resistant depression constitutes a substantial methodological oversight. Furthermore, the narrative fails to integrate a comprehensive risk‑benefit assessment that accounts for the documented cardiotoxic profile inherent to tricyclic agents, especially in geriatric cohorts. The purported cost advantage, while statistically accurate, neglects to factor in the ancillary expenses associated with electrocardiographic surveillance and potential hospitalizations resulting from adverse events. In summation, the article’s conclusions are predicated upon an incomplete evidentiary foundation and thus warrant substantial revision.
Robert Hunter
October 11, 2025 AT 11:13From a cross‑cultural perspective, it’s crucial to recognize that medication adherence can be profoundly influenced by patient beliefs about mental health, and Tofranil’s legacy may carry stigma in some communities. Providing clear educational resources alongside the pharmacologic data can bridge these gaps and promote more equitable treatment outcomes.
Shruti Agrawal
October 12, 2025 AT 15:00The guide is well‑structured and the language is clear. I especially liked the bullet points summarising key differences. It makes it easier for readers to digest complex information. Thank you for the thoughtful presentation.
Katey Nelson
October 13, 2025 AT 18:46When one contemplates the ontological interplay between chemical modulation and subjective well‑being, the discourse surrounding Tofranil transcends mere pharmacology and enters the realm of existential inquiry 😊. The dichotomy of efficacy versus side‑effects mirrors the ancient paradox of pleasure and pain, suggesting that each antidepressant is a vessel navigating the tumultuous seas of the human psyche. In this context, the cost‑effectiveness of imipramine cannot be isolated from its sociocultural imprint, for a cheap pill may still be a heavy burden if it alienates the patient from their cultural narrative. Moreover, the emphasis on QT prolongation evokes the mythic image of the heart as a fragile drum, resonating with the fear that modern medicine sometimes amplifies rather than heals. The therapeutic alliance, therefore, must be grounded in mutual respect and transparent dialogue, allowing the individual to choose not just a molecule, but a partner in their journey toward wholeness 🌟. While the article dutifully lists side‑effects, it omits the nuanced reality that a dry mouth can become a daily reminder of one’s vulnerability, subtly shaping identity. Conversely, the activation at low doses can be likened to a sunrise after a long night, offering hope to those whose insomnia has become a nocturnal prison. The meta‑analysis cited, however, is presented without a critical lens, as if the numbers alone could dictate the soul’s path. In practice, clinicians must wield both evidence and empathy, balancing statistical significance with lived experience. Ultimately, the guide serves as a map, but the traveler decides which terrain to traverse, guided by both rational calculation and the ineffable whispers of the heart.
Joery van Druten
October 14, 2025 AT 22:33I appreciate the philosophical depth you bring to the discussion, though clarity could benefit from more concise phrasing.
Melissa Luisman
October 16, 2025 AT 02:20The article misses several key contraindications that should have been highlighted.
Akhil Khanna
October 17, 2025 AT 06:06Hey folks! Just wanted to add that imipramine can be a good option for patients who need both mood lift and pain relief, especially in low dose. Also, dont forget to monitor blood pressure when combined with other meds. 😊
Zac James
October 18, 2025 AT 09:53It’s helpful to see a side‑by‑side comparison; this kind of transparent information empowers patients to make informed choices.
Arthur Verdier
October 19, 2025 AT 13:40Oh sure, the “official” guide tells us to trust the pharma‑sponsored data while conveniently ignoring the hidden agenda lurking behind every cost‑analysis. They’ll have you believe that a cheap generic like imipramine is the answer, all the while the real profit lies in the follow‑up appointments, ECGs, and the inevitable switch to a newer, pricier drug once side‑effects appear. Let’s not forget the covert collaborations between drug companies and research institutions that sculpt these “evidence‑based” recommendations to suit corporate interests. The claim that SSRIs have milder side‑effects is a lie perpetuated by marketing departments eager to push their own patents. Meanwhile, the article’s quiet nod to QT prolongation is a smoke screen, because who really reads the fine print about cardiac monitoring costs? In reality, the patient is caught in a revolving door of prescriptions, each promising relief but delivering a new set of problems. The table’s neat rows mask the messy reality of polypharmacy, where drug‑drug interactions become a ticking time bomb. If you scrape beneath the surface, you’ll see that the entire treatment paradigm is designed to keep you on medications for life, ensuring a steady revenue stream. So, next time you read a “comparative guide,” remember to question whose hands are holding the pen. The truth, as always, is buried beneath layers of corporate gloss.
Breanna Mitchell
October 20, 2025 AT 17:26Great job on the guide! It’s reassuring to see such balanced information that can help people find the right fit for their mental health journey.
Alice Witland
October 21, 2025 AT 21:13Well, after wading through the exhaustive tables, I’m convinced that choosing a pill is basically a choose‑your‑own‑adventure book-except the ending is determined by your insurance.