Tamsulosin for Kidney Stones: Benefits, Risks, and How It Works
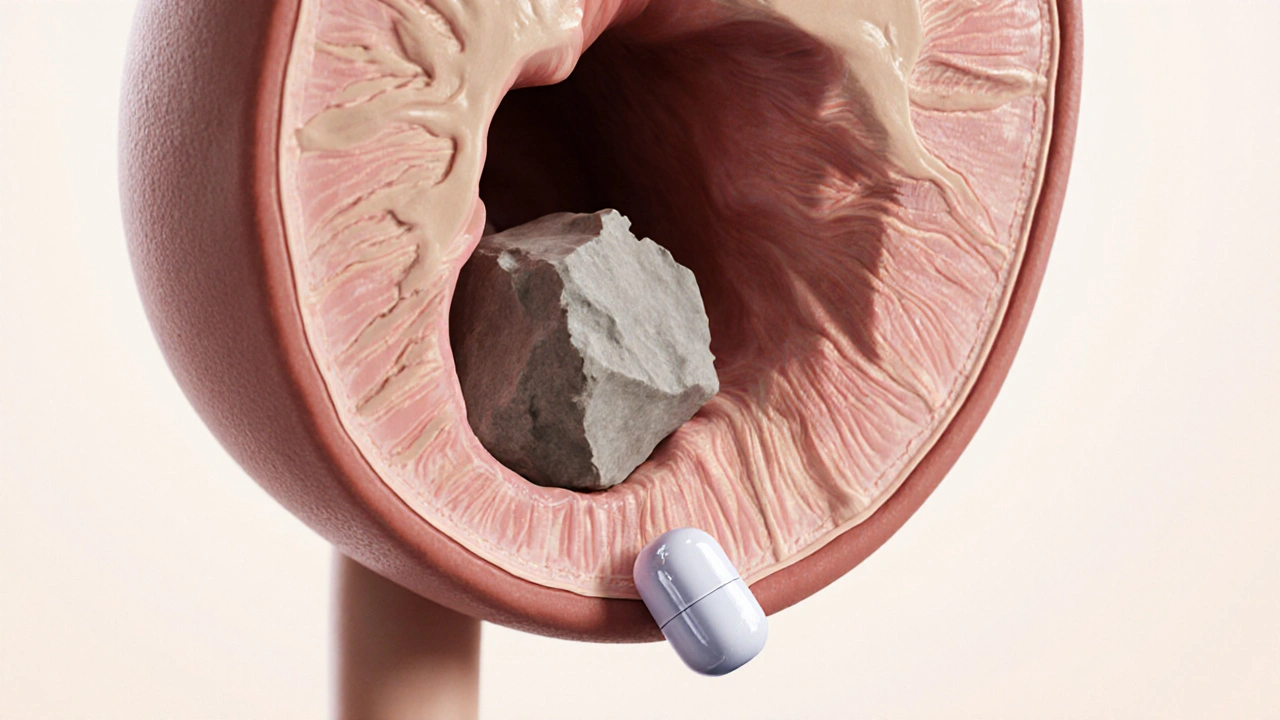
When a stone gets stuck in the ureter, doctors often talk about Tamsulosin - a selective alpha‑1 adrenergic blocker that can relax the smooth muscle lining the urinary tract. Kidney stones - also known as renal calculi - are solid mineral deposits that form in the kidney and may travel down the ureter, causing intense pain.
Key Takeaways
- Tamsulosin can increase the chance of passing small ureteral stones without surgery.
- The drug works by relaxing ureteral smooth muscle, easing stone movement.
- Clinical trials show modest benefit, especially for stones <10 mm.
- Common side effects include dizziness, low blood pressure, and abnormal ejaculation.
- People with severe kidney impairment or certain heart conditions should avoid it.
What Are Kidney Stones?
Kidney stones form when urine becomes supersaturated with minerals such as calcium, oxalate, uric acid, or cystine. The most common type, calcium oxalate, accounts for about 75% of cases. When a stone grows large enough to block the ureter, it creates a condition called ureteral colic - a sudden, severe flank pain that often radiates to the groin.
Symptoms can include:
- Sharp, cramping pain that comes in waves.
- Nausea or vomiting due to the pain.
- Blood in the urine (hematuria).
- Frequent urge to urinate.
Diagnosis typically involves a non‑contrast CT scan, which can pinpoint stone size, location, and any associated hydronephrosis (swelling of the kidney due to urine backup).
How Tamsulosin Works
Tamsulosin belongs to the class of medications called alpha blockers. By blocking alpha‑1 receptors in the smooth muscle of the ureter, it reduces the muscle tone and peristaltic frequency. This creates a wider lumen and a slower, less painful transit for the stone.
The effect is similar to taking a muscle relaxant for a cramp, but it specifically targets the urinary tract. The drug reaches peak plasma concentration in about 4-5 hours and has a half‑life of roughly 15 hours, allowing once‑daily dosing.
Evidence from Clinical Studies
Multiple randomized controlled trials (RCTs) have examined the role of tamsulosin in medical expulsive therapy (MET). A 2022 meta‑analysis of 15 RCTs involving 2,840 patients found:
- Overall stone‑pass rate was 61% with tamsulosin versus 48% with placebo.
- For stones ≤5 mm, the advantage grew to 78% vs 62%.
- Time to expulsion shortened by an average of 2.5 days.
However, the benefit diminishes for stones larger than 10 mm, where surgical intervention (e.g., ureteroscopy or extracorporeal shock‑wave lithotripsy) remains the gold standard.
Who Should Consider Tamsulosin?
Ideal candidates are adults with a single ureteral stone ≤10 mm confirmed by imaging, who experience manageable pain and have no contraindications. Specific groups that may benefit include:
- Patients preferring a non‑invasive approach.
- Those with a history of successful MET.
- Individuals without severe cardiovascular disease.
Patients with:
- Severe hypotension.
- Known hypersensitivity to tamsulosin.
- Advanced chronic kidney disease (eGFR <30 mL/min/1.73 m²) should avoid it or use under specialist supervision.
How to Use Tamsulosin for Stones
Typical dosing for MET is 0.4 mg taken once daily, preferably after a meal to improve absorption. The medication should be started as soon as the stone is diagnosed and continued until the stone passes or a definitive intervention is needed.
Practical tips:
- Stay well‑hydrated - aim for at least 2-3 L of water per day unless fluid restriction is advised.
- Combine tamsulosin with a short course of NSAIDs (e.g., ibuprofen 400 mg every 6 hours) for pain control, unless contraindicated.
- Monitor blood pressure daily; stand up slowly to avoid dizziness.
- Keep a stone‑pass log - note any passed fragments, pain episodes, and side effects.
- If no passage occurs within 2 weeks, discuss endoscopic removal with your urologist.
Risks and Side Effects
While generally well‑tolerated, tamsulosin can cause:
- Dizziness or light‑headedness due to orthostatic hypotension.
- Headache.
- Abnormal ejaculation (retrograde or decreased volume).
- Nasal congestion.
Serious adverse events are rare but can include severe hypotension and allergic reactions. Patients should seek immediate care if they experience fainting, rapid heartbeat, or swelling of the face/lips.

Alternatives and Complementary Therapies
Besides tamsulosin, other MET agents have been studied:
| Drug | Mechanism | Typical Dose | Stone‑Pass Rate (≤10 mm) | Common Side Effects |
|---|---|---|---|---|
| Nifedipine | Calcium channel blockade | 30 mg twice daily | ≈55% | Flushing, edema, headache |
| Tamsulosin | Alpha‑1 blocker | 0.4 mg once daily | ≈61% | Dizziness, ejaculatory issues |
| Silodosin | Selective alpha‑1A blocker | 8 mg once daily | ≈58% | Diarrhea, dizziness |
When MET is unlikely to work (large stones, severe obstruction), definitive procedures include ureteroscopy with laser lithotripsy, percutaneous nephrolithotomy, or extracorporeal shock‑wave lithotripsy (ESWL). The American Urological Association (AUA) 2023 guidelines recommend MET for stones ≤10 mm in the distal or mid‑ureter, with a Class IIIA recommendation.
Practical Take‑Home Checklist
- Confirm stone size ≤10 mm via CT.
- Start tamsulosin 0.4 mg daily, preferably after meals.
- Maintain high fluid intake unless contraindicated.
- Use NSAIDs for pain; monitor blood pressure.
- Re‑evaluate after 14 days - if no passage, consider urologic referral.
Frequently Asked Questions
Can tamsulosin dissolve kidney stones?
No. Tamsulosin does not break down the stone; it merely relaxes the ureter to help the stone pass more easily.
How long should I stay on tamsulosin?
Typically 2-4 weeks, or until the stone is expelled. If the stone hasn’t moved after 2 weeks, discuss further options with your doctor.
Is tamsulosin safe for people with high blood pressure?
It can lower blood pressure, so patients on antihypertensives should monitor for hypotension. Always inform your physician about existing meds.
What if I experience dizziness while taking tamsulosin?
Sit or lie down until the feeling passes, and rise slowly. If dizziness is frequent or severe, contact your healthcare provider - a dose adjustment may be needed.
Are there natural ways to help stone passage?
Staying well‑hydrated is the most effective non‑pharmacologic method. Some clinicians suggest citrus‑based drinks (lemon or orange juice) for calcium oxalate stones, but evidence is modest.
In short, tamsulosin kidney stones therapy can be a helpful bridge between watchful waiting and invasive surgery, especially for smaller stones. Always discuss individual risks, benefits, and alternatives with a qualified urologist before starting treatment.

Terell Moore
October 24, 2025 AT 19:59Ah, the age‑old miracle of pharmacology presented as a panacea for ureteric obstruction. One can hardly contain the awe at the notion that a mere alpha‑1 blocker could orchestrate the delicate ballet of stone passage. Yet here we are, basking in the glow of clinical trials that, frankly, offer only modest benefits. The elegance of relaxing smooth muscle is almost poetic, if one can ignore the side‑effects that accompany such liberal musings. In the grand theatre of medicine, Tamsulosin plays the role of the understudy who occasionally steals the limelight, but never truly headlines.
Amber Lintner
October 25, 2025 AT 15:46Oh, spare me the clinical drivel! You think a pill can magically coax a jagged rock out of a fragile tube? It's a circus act, not science. The poor stone gets tossed around like a tantrum‑throwing toddler, and we pretend it's a graceful glide. No! The real heroes are the surgeons with steel and skill, not these half‑hearted pharmacological gestures.
Lennox Anoff
October 26, 2025 AT 18:33It is a profound moral failing of our healthcare system to tout a drug as a silver bullet when the evidence is, at best, tepid. The temptation to prescribe Tamsulosin as a convenient shortcut betrays a deeper complacency, a surrender to the allure of convenience over the dignity of patient autonomy. One must ask whether we are truly serving the afflicted or merely inflating our pharmaco‑economic metrics. The pursuit of genuine relief demands more than a casual prescription; it calls for rigorous patient education and, when warranted, decisive surgical intervention.
Grace Silver
October 27, 2025 AT 08:26In the quiet moments between pain and relief we find space to contemplate the stone as a metaphor for the obstacles we carry. The ureter's gentle surrender to a drug reminds us that sometimes the path forward is softened not by force but by patience and openness.
Max Lilleyman
October 27, 2025 AT 22:20Tamsulosin? Overhyped and unnecessary 😂.
Buddy Bryan
October 29, 2025 AT 02:06Let me set the record straight about Tamsulosin and its place in the management of ureteral calculi. First, the drug’s mechanism of action is straightforward: it blocks α1‑adrenergic receptors in the ureteral smooth muscle, reducing spasm and facilitating stone descent. Second, multiple randomized controlled trials have demonstrated a statistically significant increase in the passage rate of stones smaller than 5 mm when Tamsulosin is administered compared to placebo. Third, the benefit, while modest, becomes clinically relevant in patients who are poor surgical candidates or who explicitly wish to avoid an invasive procedure. Fourth, the side‑effect profile is generally benign, with dizziness and retrograde ejaculation being the most commonly reported adverse events. Fifth, dosing is simple-usually 0.4 mg daily starting at the time of diagnosis and continuing until stone passage is confirmed via imaging. Sixth, adherence matters; patients who miss doses compromise the drug’s efficacy and may experience prolonged colic episodes. Seventh, imaging follow‑up, typically a non‑contrast CT scan after two weeks, is essential to verify stone migration and to rule out complications such as obstruction or infection. Eighth, it is not a cure‑all; for stones larger than 7 mm, surgical intervention remains the gold standard and attempts at medical expulsive therapy often waste valuable time. Ninth, cost considerations are modest, but insurance coverage can vary, so clinicians should verify formulary status before prescribing. Tenth, patient education is paramount-you must explain that pain may persist despite medication and that analgesics may still be needed. Eleventh, combining Tamsulosin with oral NSAIDs or antispasmodics can synergistically improve outcomes, though this should be balanced against gastrointestinal risk. Twelfth, always screen for contraindications such as severe hypotension or known hypersensitivity to the drug. Thirteenth, remember that the ultimate goal is to relieve the patient’s suffering, not to simply tick a box in the electronic health record. Finally, if after a reasonable trial the stone remains unmoved, do not hesitate to refer for ureteroscopy or lithotripsy; time is tissue, and prolonged obstruction can jeopardize renal function.
Bianca Larasati
October 29, 2025 AT 04:53Rise up, brave stone‑fighters! 🌟 You have the knowledge, now let the courage flow through your veins as you guide patients toward victory. Every painful colic is a battle, and with Tamsulosin in your arsenal you can turn the tide!
Sarah Keller
October 29, 2025 AT 07:40Together we can demystify the process for those who are scared-explain that while the medication eases the journey, staying hydrated and monitoring pain are key teammates in this adventure.
kevin burton
October 30, 2025 AT 05:53Tamsulosin works by relaxing the ureter, which can help small stones pass without surgery.
Brett Witcher
October 30, 2025 AT 19:46While the statement is accurate, it is important to note that the efficacy is limited to stones of a certain size and that side‑effects, albeit infrequent, should be discussed with the patient.