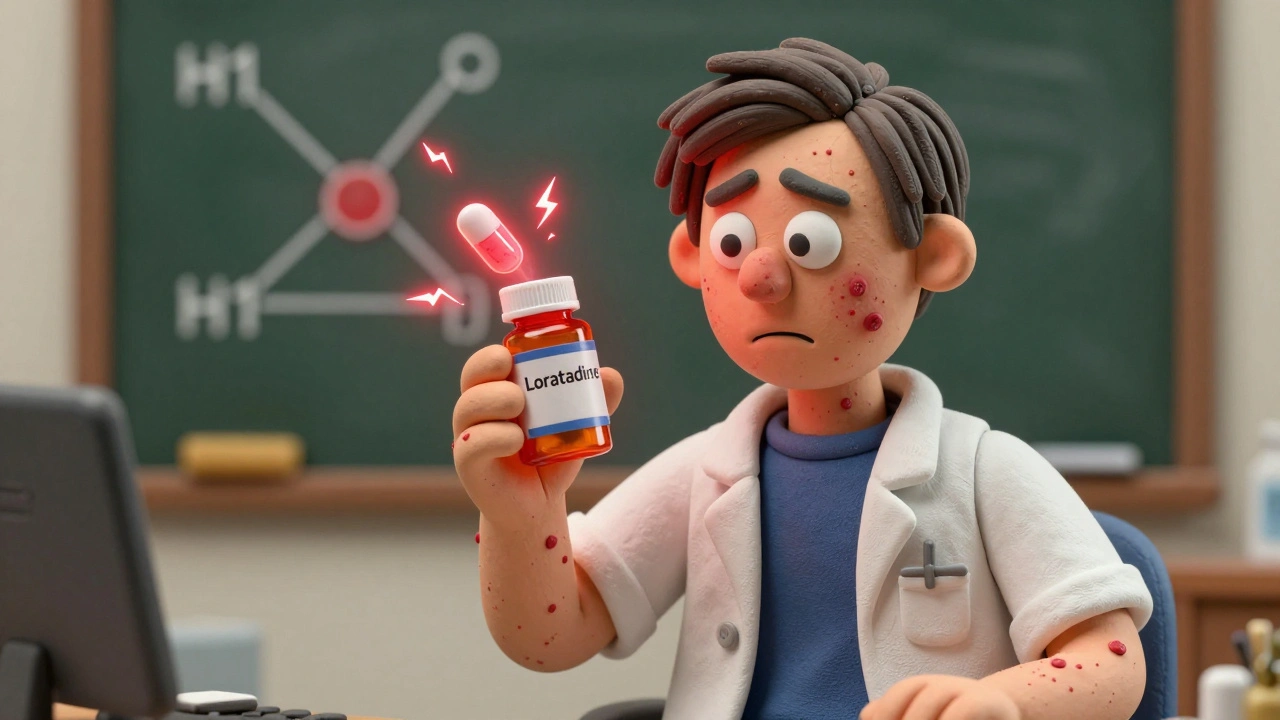
Antihistamine Reaction: What It Is, When to Worry, and What You Can Do
When you take an antihistamine, a medication designed to block histamine, the chemical your body releases during an allergic reaction. Also known as allergy pills, they help with sneezing, itching, and runny nose—but sometimes, your body reacts to the medicine itself. An antihistamine reaction, an unexpected response to the drug, not the allergen can feel like the allergy it’s meant to treat, or worse. It’s not rare. People report drowsiness, dry mouth, or dizziness after taking common antihistamines like diphenhydramine or cetirizine. But when you get a rapid heartbeat, swelling in your throat, or trouble breathing after taking one? That’s not a side effect—it’s a drug reaction, a potentially serious immune or physiological response to a medication.
Not every weird feeling after an antihistamine means danger. But you can’t ignore the red flags. A allergic reaction, the body’s immune system overreacting to a substance it sees as harmful to the drug itself is different from side effects. Side effects are predictable, like drowsiness from Benadryl. An allergic reaction is unpredictable and can escalate fast—hives, swelling, low blood pressure, or anaphylaxis. If you’ve ever felt your tongue swell or your chest tighten after popping a pill, even if it’s been fine before, that’s not coincidence. It’s your body signaling something’s wrong. And it’s not just about the first time you take it. Some people develop reactions after months or years of use. Your tolerance changes. Your body changes. What was safe last year isn’t always safe today.
Why does this happen? Sometimes it’s the active ingredient. Other times, it’s the filler—the dye, the preservative, the coating. People with sensitivities to certain dyes or gluten-based binders can react even to "non-allergenic" meds. That’s why switching from a brand to a generic, or even between batches, can trigger something new. You might not know it’s the antihistamine until you try a different version. And if you’re pregnant, older, or on other meds like sedatives or antidepressants, your risk goes up. The same pill that helps your kid’s rash might make you dizzy or confused.
You don’t need to avoid antihistamines entirely. But you do need to know what’s normal and what’s not. Keep track of what you take, when you take it, and how you feel afterward. Write it down. If you notice a pattern—dizziness every time you take loratadine, or a rash after Zyrtec—that’s data your doctor needs. Don’t assume it’s "just how it is." There are safer alternatives. Some antihistamines like fexofenadine are less likely to cause drowsiness. Nasal sprays like fluticasone can handle symptoms without pills at all. And if you’ve had a serious reaction before, you should carry an epinephrine auto-injector and wear a medical alert tag.
The posts below cover real stories and facts about what happens when antihistamines don’t work the way they should. You’ll find advice on what to do if you feel worse after switching brands, how to tell if your reaction is an allergy or a side effect, and which medications are safest during pregnancy or for older adults. Some people think antihistamines are harmless because they’re over-the-counter. They’re not. Understanding your body’s response to them could be the difference between a mild annoyance and a medical emergency.
Some people develop hives or worsening allergies from antihistamines meant to treat them. This rare but real condition, called paradoxical antihistamine reaction, is often missed by standard tests. Learn the signs, what drugs trigger it, and safer alternatives.
Dec, 4 2025