Red Flags in Drug Interactions: Combinations Your Pharmacist Should Question

Drug Interaction Checker
Check Your Medication Combinations
This tool identifies dangerous combinations mentioned in the article that can cause serious health risks or death. Note: This is for informational purposes only and does not replace professional medical advice.
Remember: This is not medical advice. Always consult with your healthcare provider before making any changes to your medications.
Every year, tens of thousands of Americans end up in the emergency room because of drug interactions that should have been caught. Not because the medications were wrong, but because no one stopped to ask: What happens when these two are taken together?
These Five Combinations Can Kill You
Some drug pairs are like gasoline and a match. They don’t just cause mild side effects-they can trigger heart attacks, kidney failure, or sudden death. The Chicago Tribune’s 2016 investigation tested five dangerous combinations that pharmacies missed more than half the time. Here’s what you need to know.
- Tizanidine + Ciprofloxacin: One is a muscle relaxer, the other an antibiotic. Together, they shut down a key liver enzyme (CYP1A2), causing sudden loss of consciousness. People have collapsed while walking, driving, or even standing in line at the grocery store.
- Colchicine + Verapamil: Used for gout and high blood pressure, this combo blocks a protein that clears toxins from the body. Result? Colchicine builds up to deadly levels-leading to muscle breakdown, organ failure, and death.
- Simvastatin + Clarithromycin: This is one of the most common mistakes. Simvastatin lowers cholesterol. Clarithromycin fights infections. But together, they trigger rhabdomyolysis, a condition where muscle tissue melts into the bloodstream, crushing the kidneys. Creatine kinase levels can spike over 10,000 U/L-normal is under 200.
- Clarithromycin + Ergotamine: Ergotamine treats migraines. Clarithromycin is a common antibiotic. Combined, they cause ergotism: severe blood vessel spasms, gangrene in fingers and toes, and sometimes amputation or death.
- Birth Control + Griseofulvin: This one is sneaky. Griseofulvin, an antifungal for nail fungus, speeds up how fast your body breaks down estrogen. Birth control fails. Pregnancy rates jump above 30%. And if you get pregnant while on this combo, your baby could be born with serious birth defects.
These aren’t rare cases. They’re predictable. And they happen every day.
Why Your Pharmacist Might Not Catch Them
You might assume your pharmacist checks every interaction. But here’s the truth: they’re drowning in alerts.
Computer systems flag every possible drug interaction-even ones that are harmless. A pharmacist might get 50 warnings for a single prescription. Most are low-risk: “This drug might cause mild nausea if taken with that one.” After seeing the same alerts 20 times a day, the brain stops paying attention. It’s called alert fatigue.
Professor John Horn from the University of Washington School of Pharmacy studied this. He found that in 52% of cases, pharmacists missed life-threatening combinations-not because they were careless, but because the system was designed to scream too loudly.
Imagine a fire alarm that goes off every time someone opens a window. You’d eventually ignore it. That’s what’s happening in pharmacies.
Warfarin and Amiodarone: A Silent Killer
Warfarin (Coumadin) is a blood thinner used by millions to prevent strokes. Amiodarone is a heart rhythm drug. Together, they’re a recipe for internal bleeding.
Amiodarone blocks the liver enzymes that break down warfarin. That means warfarin builds up in your blood. Your INR-a measure of how long it takes your blood to clot-can spike overnight. One patient might be fine at INR 2.5, then suddenly hit 8.0. That’s a 200% increase in bleeding risk.
The American Academy of Family Physicians says: if you’re prescribed amiodarone while on warfarin, your dose must be cut by 30-50% right away. You need weekly INR checks for at least a month. Yet many pharmacies don’t flag this unless the system is customized. And most aren’t.
And it’s not just amiodarone. Some statins-like simvastatin, lovastatin, and fluvastatin-also interfere with warfarin. Atorvastatin and pravastatin? Much safer. But unless your doctor and pharmacist know this, you’re playing Russian roulette with your blood.

Digoxin and Verapamil: The Heart’s Trap
Digoxin (Lanoxin) helps weak hearts pump better. Verapamil slows your heart rate. Together, they’re a double hit.
Verapamil reduces how fast your kidneys clear digoxin. It also cuts down how much gets removed through the bile. Result? Digoxin levels jump by 60-75%. That’s not just a side effect-it’s toxicity.
Signs? Nausea, vomiting, blurry vision, confusion, and a dangerously slow heartbeat. In severe cases, it causes heart block-where your heart skips beats so badly it stops.
Doctors are supposed to monitor EKGs and digoxin blood levels. But if your pharmacist doesn’t flag it, and your doctor doesn’t check, you could be walking around with a ticking time bomb in your chest.
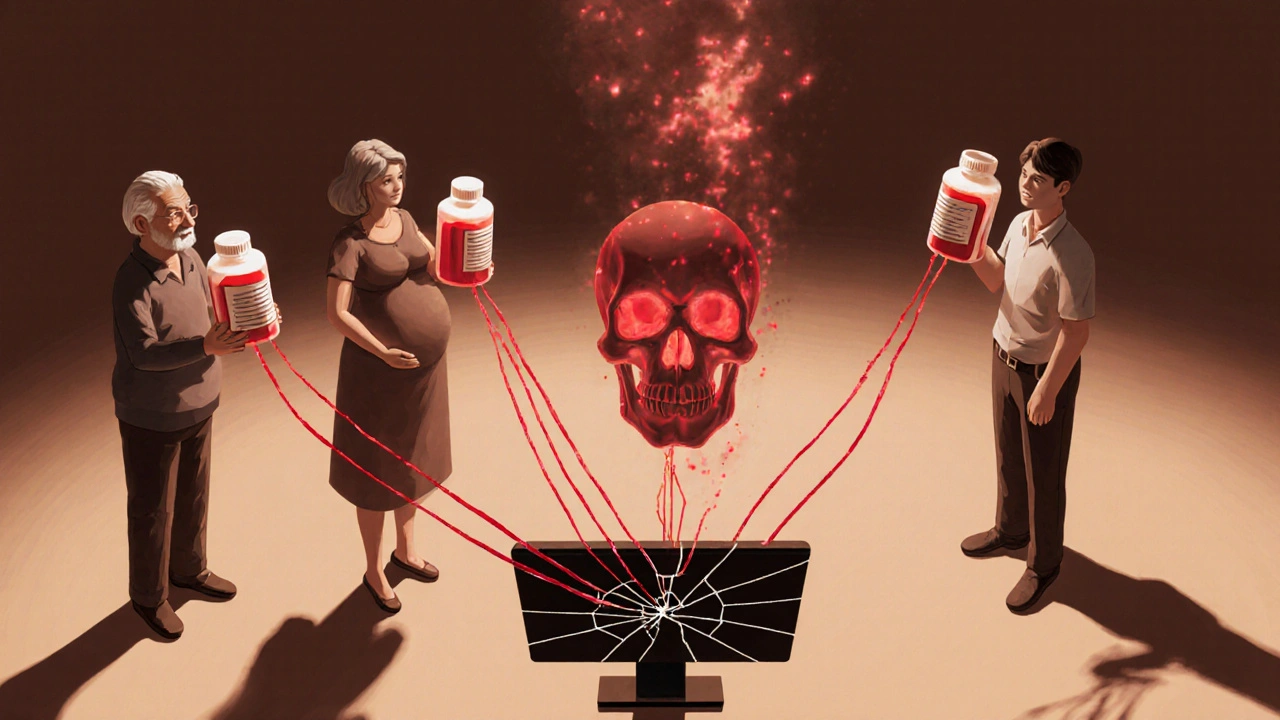
Who’s Most at Risk?
It’s not just about the drugs. It’s about who’s taking them.
- Older adults: The average 70-year-old takes 4.5 prescription drugs daily. The FDA says they account for 35% of all serious adverse drug events. One extra pill can tip the balance.
- People with kidney or liver disease: These organs clear drugs from your body. If they’re weak, even normal doses become toxic.
- Pregnant women: Some drugs, like griseofulvin, don’t just fail birth control-they cause birth defects. Yet many women don’t realize their antifungal treatment could endanger their pregnancy.
- Those on multiple specialists: One doctor prescribes a new painkiller. Another adds a sleep aid. A third gives an antibiotic. No one talks to each other. The pharmacist is the last line of defense.
And here’s the worst part: many of these deaths are misclassified. A patient dies of a heart attack. The chart says “cardiac arrest.” No one looks back to see if it was caused by a drug combo that was never flagged.
What You Can Do Right Now
You can’t fix the system. But you can protect yourself.
- Keep a written list of every medication you take-including over-the-counter pills, vitamins, and supplements. Bring it to every appointment.
- Ask your pharmacist: “Are any of these drugs dangerous to take together?” Don’t wait for them to speak up. Ask directly.
- Know your high-risk drugs: If you’re on warfarin, digoxin, simvastatin, or birth control, be extra careful with antibiotics like clarithromycin or antifungals like griseofulvin.
- Use one pharmacy: If you get prescriptions from multiple places, your meds aren’t being tracked as a whole. One pharmacy can see everything.
- Check for updates: If your doctor changes one drug, ask if it affects the others. A new painkiller might cancel out your blood pressure med.
And if your pharmacist says, “It’s fine,” ask: “Is this on the list of combinations that can cause death?” If they hesitate, walk out and call another pharmacy. Better safe than sorry.
Why This Keeps Happening
Pharmacies are under pressure. The average prescription is processed in 2.3 minutes. That’s not enough time to read a patient’s full history, check for interactions, and explain risks.
Big chains like CVS and Walgreens promised changes after the Tribune’s report. Some improved their alert systems. Some hired more staff. But 30% of community pharmacies still don’t have smart systems that filter out low-risk alerts.
And the problem is getting worse. By 2030, the National Academy of Medicine predicts a 27% rise in drug-related harm-because more people are on more drugs, and our systems aren’t keeping up.
Artificial intelligence is being tested to predict interactions based on age, weight, kidney function, and genetics. But until those tools are standard, you’re the most important safety net.
Final Warning: Don’t Assume It’s Safe
Medications aren’t harmless. Even common ones-like ibuprofen, antibiotics, or cholesterol pills-can turn deadly when mixed.
There’s no app that replaces human vigilance. No computer that knows your history better than you do. And no pharmacist who can catch everything if they’re buried under 50 false alarms.
If you’re taking more than three prescriptions, you’re at risk. If you’re over 65, you’re at higher risk. If you’ve ever had a strange reaction to a new drug, you’re at the highest risk.
Don’t wait for someone else to protect you. Ask. Double-check. Speak up. Your life might depend on it.
What are the most dangerous drug combinations I should watch out for?
The most dangerous combinations include simvastatin with clarithromycin (risk of muscle breakdown and kidney failure), tizanidine with ciprofloxacin (sudden loss of consciousness), colchicine with verapamil (toxic buildup leading to organ failure), clarithromycin with ergotamine (deadly blood vessel spasms), and birth control with griseofulvin (contraceptive failure and birth defects). Warfarin with amiodarone or certain statins also raises bleeding risk significantly.
Why do pharmacists miss dangerous drug interactions?
Pharmacists often face alert fatigue-hundreds of computer warnings per day, most of which are low-risk. When systems don’t prioritize life-threatening interactions, important alerts get ignored. Many pharmacies still use outdated systems that flag every possible combo, not just the dangerous ones.
Can over-the-counter meds cause dangerous interactions?
Yes. Even common OTC drugs like ibuprofen, naproxen, or cold medicines with decongestants can interact with blood thinners, blood pressure meds, or antidepressants. St. John’s Wort can make birth control fail. Antacids can reduce absorption of antibiotics. Always tell your pharmacist everything you take-even supplements.
How can I make sure my pharmacist checks my meds properly?
Use one pharmacy for all your prescriptions. Bring a written list of every medication, including vitamins and herbs. Ask directly: “Are any of these drugs dangerous to take together?” If they say it’s fine but you’re unsure, get a second opinion from another pharmacist. Don’t rely on silence as safety.
What should I do if I think I’m having a drug interaction?
Stop taking the suspected combination immediately. Call your doctor or pharmacist. If you have symptoms like confusion, chest pain, muscle weakness, unusual bleeding, or fainting, go to the ER. Don’t wait. Drug interactions can escalate fast-especially in older adults or those with kidney or liver problems.

JD Mette
November 22, 2025 AT 21:29This post hit me hard. My dad passed away last year after a routine antibiotic prescription. The coroner never mentioned drug interactions, but looking back, he was on warfarin and clarithromycin. No one asked. No one flagged it. I wish I’d known then what I know now.
Olanrewaju Jeph
November 23, 2025 AT 08:33Excellent breakdown. The pharmacokinetic mechanisms described are accurate and clinically significant. The CYP1A2 inhibition by ciprofloxacin leading to tizanidine toxicity is a well-documented case in the Journal of Clinical Pharmacology. Systemic alert fatigue is a documented phenomenon in healthcare informatics literature. This needs to be mainstreamed.
Karla Morales
November 23, 2025 AT 18:04Oh my GOD. 😱 I just realized I’ve been taking simvastatin and clarithromycin together for three months. My muscles have been aching like crazy. I thought it was just aging. I’m calling my pharmacy RIGHT NOW. Thank you for saving my life. 🙏
Javier Rain
November 24, 2025 AT 22:12Listen - this isn’t just about pharmacists. It’s about YOU taking charge. I used to wait for doctors to fix everything. Then I started carrying a laminated list of my meds in my wallet. Now I ask every single pharmacist: ‘Is this combo lethal?’ They don’t like it. But I’m alive. You will be too. Don’t be passive. Be loud.
Laurie Sala
November 26, 2025 AT 21:07Wait… wait… wait… so you’re saying pharmacies are FAILING people?!!?!?!?!?!?!? I’m not surprised. I’ve been to CVS three times this year - each time, the pharmacist was on their phone. I swear, they don’t even look at the screen. This is a national crisis. We need lawsuits. We need protests. We need to burn down the system.
Matthew Mahar
November 26, 2025 AT 23:28Man… I didn’t even know griseofulvin could mess with birth control. I took it last year for toenail fungus and didn’t tell my OB-GYN. I’m lucky I didn’t get pregnant. I’m going to print this out and tape it to my fridge. This is life-or-death stuff. Thanks for writing this.
John Mackaill
November 27, 2025 AT 08:59I’ve worked in community pharmacy for 17 years. The system is broken. We get 80 alerts per script. 75 are ‘possible drowsiness with grapefruit.’ The one about digoxin and verapamil? Buried. I’ve lost count of how many times I’ve called a doctor to say, ‘This combo could kill.’ Most don’t care. We’re not villains. We’re drowning.
Adrian Rios
November 28, 2025 AT 00:37Let’s be real - this isn’t just about drugs. It’s about a healthcare system that treats patients like data points. You get one prescription from your cardiologist, another from your rheumatologist, another from your dermatologist, and no one talks. The pharmacist? They’re the last person in line with a broken flashlight trying to see in the dark. We need integrated EHRs. We need mandatory interaction checks. We need to stop blaming the pharmacist for a system designed to fail. And if you’re on more than three meds? You’re not just a patient - you’re a walking minefield. Learn your meds. Know your risks. Speak up. Even if they roll their eyes. Even if they’re busy. Even if you feel stupid. Your life isn’t a suggestion. It’s non-negotiable.
Casper van Hoof
November 29, 2025 AT 14:08The tragedy here is not merely pharmacological, but epistemological: the commodification of care has rendered the physician-patient-pharmacist triad into a transactional pipeline. The algorithmic overstimulation of clinical decision support systems produces a kind of learned helplessness - a phenomenon analogous to the paradox of choice, wherein the abundance of warnings renders the critical ones imperceptible. One cannot save a life if one is conditioned to ignore the alarm.
Richard Wöhrl
December 1, 2025 AT 04:52Important note: Amiodarone’s half-life is 58 days. That means even if you stop it, it’s still in your system for months. If you’re on warfarin and your cardiologist switches you off amiodarone - DON’T assume your INR is safe. Keep checking for 3 months. I’ve seen patients bleed out because they thought ‘off the drug’ meant ‘safe.’ Also: St. John’s Wort + SSRIs = serotonin syndrome. Always mention supplements. Always.
Pramod Kumar
December 2, 2025 AT 04:27Bro, this is the real deal. In India, people take 10 pills a day - antibiotics, painkillers, ayurvedic stuff, all mixed with chai. No one checks. My uncle died from colchicine + verapamil. They called it ‘sudden heart failure.’ No one knew he had gout. We need a national awareness campaign. Maybe a poster in every pharmacy: ‘This combo kills. Ask.’
Brandy Walley
December 2, 2025 AT 13:30Ugh this is so dramatic. People die from everything. You wanna live? Stop taking pills. Just stop. I’ve been on 5 meds and I’m fine. Your body is designed to handle stuff. Stop being paranoid. Also, why do you even trust pharmacists? They’re just minimum wage workers. Get a real doctor. Or don’t take meds at all. Simple.
shreyas yashas
December 3, 2025 AT 05:20My mom’s on digoxin and verapamil. She gets dizzy every time she stands up. I told her to ask her doc. She said, ‘It’s fine, they’ve been doing this for years.’ I’m taking her to a new cardiologist next week. This post saved her life. Thanks.
Bryson Carroll
December 5, 2025 AT 01:46Wow what a guilt trip. So now I’m supposed to feel bad for taking my meds? Who died? Oh right - someone who didn’t do their own research. You think your pharmacist is your mom? Get a brain. If you can’t read the label, don’t take the pill. End of story.
Adrian Rios
December 5, 2025 AT 17:02Brandy - you’re the reason this system is broken. You think ignorance is strength. You think ‘just stop taking pills’ is a solution. That’s not freedom. That’s suicide by neglect. Your attitude kills people. And you don’t even know it.