Lipitor: Cholesterol Lowering Tips, Side Effects, and Dosages Explained

One out of every four American adults over 40 is on a statin, and Lipitor tops the list. Back at the turn of the millennium, you’d see TV commercials for Lipitor so often you could quote Dr. Robert Jarvik’s pitch in your sleep. Maybe you’re thinking about starting it because your doctor’s waving around a cholesterol reading of 260. Or maybe your bottle already stands next to your toothbrush and you’re wondering if that muscle twitch is something to worry about. Whatever landed you here, Lipitor’s story is tangled up with millions of households, medical breakthroughs, and a pile of surprising facts that go way beyond cholesterol.
What is Lipitor and How Does It Work?
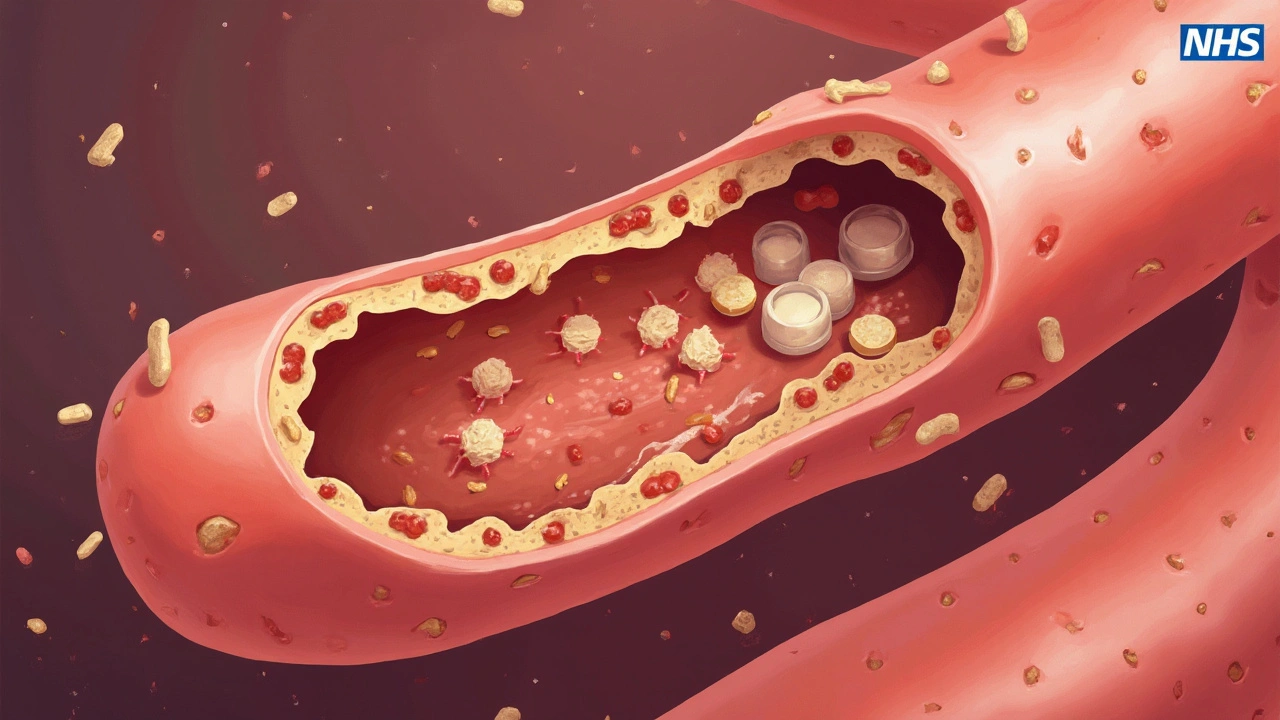
Lipitor (atorvastatin calcium) isn’t just a medication; it’s the most prescribed statin worldwide, and at one time, the best-selling drug ever made. It hit pharmacy shelves in 1997, quickly changing the way doctors fought heart attacks and strokes. The science? Lipitor blocks an enzyme in your liver called HMG-CoA reductase—think of it like a master switch for cholesterol production. When the switch stays off, your body churns out less LDL (“bad”) cholesterol. Less bad cholesterol means less plaque gumming up your arteries. That lowers your risk for a whole lineup of serious trouble: heart attacks, strokes, and even certain circulatory problems in your legs.
What’s wild is that Lipitor doesn’t just bring your cholesterol numbers down; it can trim your risk of a heart attack by up to 36%. Several clinical trials, like the TNT (Treating to New Targets) study, found patients taking Lipitor had fewer fatal heart events and less need for emergency procedures, even if their cholesterol wasn’t sky-high to begin with. Doctors often ramp up the dose, aiming for LDL levels below 70 for folks who’ve already had a heart attack. The typical starting dose is 10 or 20 mg once daily, but it goes as high as 80 mg if your arteries are really protesting.
Lipitor also has a bit of a domino effect on other blood fats, lowering triglycerides by 10-30% and sometimes nudging HDL (“good” cholesterol) up. All these effects kick in within two weeks, though the full impact can take six weeks. By then, most folks see their LDL numbers drop by at least 40%. For some, that drop is even steeper. And unlike older meds that caused flushing or stomach pain, Lipitor’s side effects tend to be milder for most people. Still, all statins share a certain “mystique”: nobody feels different when they swallow one, so it’s easy to wonder if anything real is happening.
Who Should Take Lipitor, and Who Should Avoid It?
Doctors hand out Lipitor like candy to people with high LDL cholesterol (above 130 mg/dL), folks who’ve already had a heart attack or stroke, and those with diabetes or a strong family history of early heart disease. The 2023 American College of Cardiology guidelines call it “first-line protection” for adults aged 40-75 with a 10-year risk of heart disease over 7.5%. So, if your parent landed in the hospital for a bypass in their fifties, you probably land in “statin territory” long before your senior discounts kick in. Even if your LDL cholesterol barely sneaks above “normal,” certain risk factors (high blood pressure, smoking, diabetes) can make Lipitor worth considering.
Now, not everyone should jump aboard the Lipitor train. Allergic to statins? Pregnant or trying to get pregnant? Dealing with active liver disease? Those are hard no’s. Even heavy drinkers get a warning—since Lipitor works in the liver, doctors keep an extra eye out for signs of damage. The FDA says kids as young as 10 could take Lipitor for rare genetic cholesterol disorders, but most people under 18 or over 75 won't be prescribed it unless there’s a really clear reason. Some folks bounce off Lipitor because of side effects (more on that coming up), but for most, the numbers say the longer you stick with it, the more you’ll avoid trouble down the line.
Here’s a quick look at the kind of people who should talk to their doctor before starting:
- History of muscle problems on statins
- Severe kidney disease (can increase drug levels in blood)
- Using certain antibiotics or antifungal drugs (interaction alert!)
- Serious thyroid issues
- Poor memory or confusion (rare, but possible statin side effect)
And, if you’re pregnant, Lipitor’s just not safe for a developing baby. Doctors will swap in other treatments or pause statins entirely until after pregnancy and breastfeeding. Always something fun, right?
Common Side Effects, Hidden Risks, and How to Handle Them
Most people pop their Lipitor and get on with their day. But if you ever catch yourself Googling “lipitor muscle pain at night,” you’re not alone. Muscle aches are probably the biggest reason people quit statins—anywhere from 5% to 10% of patients report them. The pain usually isn’t sharp but feels nagging, like you pulled something while wrestling a stubborn lawnmower. For most, it fades after a few weeks or months. If your muscles feel weak or your pee looks dark (like cola), that’s a red flag—see your doctor right away. That could mean a rare but serious muscle breakdown called rhabdomyolysis.
Far more common are everyday annoyances: headaches, stomach cramps, diarrhea, joint pain, or trouble sleeping. My wife Briony once called it “the full bingo card of middle age” when her doctor ran through the list. Fortunately, these effects are usually mild, and many go away as your body adjusts. Every three to six months, doctors monitor your liver enzymes and cholesterol, just to make sure nothing’s drifting off target. In less than 2% of people, Lipitor can raise blood sugar enough to nudge them into diabetes, most often in folks who were close to the edge to begin with. Here’s the thing: the risk of heart attack drops by way more than the tiny increase in diabetes risk, so doctors almost always stay the course.
Every so often, reports pop up about memory fog or mood swings. Hard scientific proof is thin, but if your thinking feels off, don’t tough it out on your own. Talk with your doctor about lowering the dose, switching to another statin, or even taking a “statin holiday.” (That’s when you pause statins for a few weeks with your doctor’s guidance to see if things improve.) If you’re curious about numbers, check out the table below for recent data from the National Health and Nutrition Examination Survey:
| Side Effect | Frequency (%) | Notes |
|---|---|---|
| Muscle aches/pain | 7-10 | Often mild, improves with dose reduction or switch |
| Liver enzyme increase | 0.7-2 | Usually mild, reversible |
| Digestive upset | 3-5 | Cramping, nausea, diarrhea |
| Increased blood sugar | 1-2 | More likely if pre-diabetic |
| Serious muscle injury | <0.1 | Very rare (rhabdomyolysis) |
Simple tips help a lot: Take your dose at the same time each day (usually bedtime is easiest on the stomach). If side effects bug you, try switching from Lipitor to another statin, as not all act exactly the same. Avoid grapefruit or grapefruit juice—they mess with the enzymes that break down Lipitor, spiking your blood levels and risk of side effects. Stay hydrated, especially if you’re working out hard. And get your annual bloodwork—nothing beats hard numbers for peace of mind.
Making Lipitor Work for You: Tips for Best Results
Here’s where rubber meets the road. Just taking Lipitor isn’t enough to dodge a heart attack if the rest of your lifestyle is tripping up your arteries. Diet, exercise, and quitting cigarettes all pull more weight together than any single pill. Load your plate with fiber—think oats, beans, apples—and swap that burger for a handful of walnuts now and then. Regular walks or biking make both the drug and your heart stronger. If you’re overweight, even dropping 10 pounds can drop your LDL cholesterol nearly as much as doubling your Lipitor dose. Managing stress matters, too: chronic anxiety bumps up your blood pressure and your risk.
People often ask if vitamins or supplements can replace Lipitor. The short answer? Nope—not if you’re in the high-risk club. Red yeast rice, garlic, niacin, and plant stanols have tiny effects compared to statins, and some interact dangerously with Lipitor. Stick with what works until you’ve talked to a real doctor.
Some tips for taking Lipitor like a pro:
- Take it at the same time each day (try linking it to brushing your teeth)
- Watch out for other prescriptions that interact (like certain antibiotics, antifungals, or HIV drugs)
- Skip grapefruit juice entirely
- Let your doctor know about any strange muscle pain, weakness, or memory changes
- Don’t stop Lipitor suddenly without talking to your doctor—your cholesterol levels can climb back up fast
- Check your cholesterol, liver, and blood sugar once or twice a year while on the drug
A lot of my friends who start Lipitor griped at first—mostly about taking a daily pill—but after they saw their cholesterol drop 40 points, it turned into a running joke. "Remind me why I ever worried about my liver when my arteries got a 10-year lease on life?" Even my pharmacist throws in, “Statins keep us all in business—but mostly out of the hospital.” That’s not a bad deal, especially if you’ve got little kids, world travel dreams, or just want to see your team win one more time. If you’ve got questions about Lipitor, don’t be shy with your provider. You’re not just keeping your numbers in check—you’re giving your heart some serious backup, one day at a time.

Herbert Lui
June 15, 2025 AT 06:55So Lipitor’s the new coffee-everyone’s got a bottle, nobody talks about how weird it is that we’re all just quietly medicating our biology into compliance.
It’s not a drug, it’s a lifestyle accessory. You swallow it like a vitamin, stare at your reflection in the bathroom mirror, and wonder if you’re healthier-or just better at pretending.
My grandpa took it for 12 years. Never felt a thing. Died of a fall at 89. The statin didn’t save him. The fact that he still walked to the corner store did.
Maybe the real miracle isn’t the cholesterol drop. It’s that we’ve convinced ourselves that numbers on a lab sheet are more real than the way we breathe, move, or feel at 3 a.m.
Cholesterol’s not the enemy. Fear of dying before your grandchildren graduate is.
And Lipitor? It’s just the most expensive Band-Aid we’ve ever invented that also makes your legs feel like wet cement.
But hey-I’ll take the cement legs if it means my kid doesn’t have to bury me at 58.
So I pop it.
And I don’t ask questions.
Because sometimes, the most radical thing you can do is just keep showing up.
Even if you’re just a ghost with a prescription.
Nick Zararis
June 15, 2025 AT 23:43Just a quick note: if you're experiencing muscle pain, don't just assume it's 'normal'-get your CK levels checked, please!; also, avoid grapefruit-yes, it's still a thing-and if you're on antibiotics like clarithromycin? Talk to your pharmacist-seriously, don't wing it.; liver enzymes? Monitor every 3-6 months; and if your doctor doesn't bring it up, ask-because you're not just a number, you're a person with a body that deserves attention.; also, statins aren't magic-they're tools.; use them wisely.
Sara Mörtsell
June 15, 2025 AT 23:51Everyone’s acting like Lipitor’s some kind of miracle cure when really it’s just corporate medicine’s greatest hit-pharma made billions off our fear of death and our refusal to eat vegetables.; I’ve seen people on Lipitor who still eat fried chicken every day and think they’re ‘doing their part’.; You don’t get to medicate your way out of a life built on soda and Netflix.; The real side effect? Complacency.; The real risk? Not the muscle pain-it’s believing you’ve done enough just because you swallowed a pill.; So yeah-I’m not judging your choice.; I’m judging the system that sold you this lie as if it were salvation.
Rhonda Gentz
June 16, 2025 AT 19:21I’ve been on Lipitor for seven years. I didn’t feel anything at first. No energy boost. No dramatic change. Just… quieter. Less anxiety about heart attacks. Less dread when I saw my dad’s EKG from 2012.
It’s not about being healthy. It’s about not being a statistic.
I don’t talk about it much. I don’t need to. It’s just there. Like my glasses. Like brushing my teeth.
Some days I wonder if I’d be better off without it.
Then I remember the hospital room.
The beeping.
The silence after the doctor said, ‘We caught it early.’
And I take it again.
Because sometimes, peace isn’t loud.
It’s just a pill.
And a quiet life.
Alexa Ara
June 17, 2025 AT 08:53Hey, if you're thinking about starting Lipitor-just know you're not alone. I was terrified too. But my cardiologist broke it down so simply: ‘It’s not about being perfect. It’s about being protected.’
My numbers were borderline, but my family history? Yeah. That tipped the scale.
Side effects? I had a little stomach upset for the first week. Then nada.
And honestly? The peace of mind? Priceless.
Don’t let fear stop you from doing something that could give you more years with your people.
You’ve got this.
And if you’re nervous? Ask your doctor for a lower dose first. No shame in starting slow.
Small steps, big impact.
Olan Kinsella
June 17, 2025 AT 21:10You think you’re safe because you take a pill?
Let me tell you about my cousin in Lagos-he took Lipitor, stopped eating yams, started eating processed bread, and died at 47 of a stroke.
They say it’s the drug.
No.
It’s the lie.
The lie that you can buy your way out of a broken system.
It’s not the statin that kills.
It’s the silence after you swallow it.
The silence when you stop asking why your food is poison.
Why your doctor doesn’t ask about your stress.
Why your country sells you medicine instead of meals.
So yeah.
Take the pill.
But don’t forget to scream.
Because pills don’t fix systems.
People do.
Kat Sal
June 18, 2025 AT 10:16Just want to say-this post is so helpful and I’m so glad someone laid it all out like this.
I was on Lipitor for a year and had a weird headache for a month-I thought it was stress, but my doctor said it was likely the statin and we dropped the dose from 20 to 10 mg.
Boom. Headache gone.
Cholesterol still down.
So don’t panic if something feels off-sometimes it’s just a tweak away from feeling like yourself again.
And if you’re scared? Talk to someone. Call your pharmacist. Text a friend who’s been there.
You’re not alone in this.
And you’re doing great just by showing up and learning.
Rebecca Breslin
June 19, 2025 AT 10:02Wow, this post is basically a textbook chapter. I’m impressed.
But let me add something-did you know that in Canada, they don’t even prescribe Lipitor as first-line anymore? We use rosuvastatin because it’s more potent and has fewer interactions.
Also, the 80mg dose? Only for high-risk patients. Most people don’t need it.
And if you’re over 75? The data is mixed-some studies show no benefit, some show increased fall risk.
So yes, Lipitor’s great-but context matters.
Don’t just follow the trend.
Ask your doctor: ‘Is this right for MY risk profile?’
Not just ‘Is it the most prescribed?’
Because medicine isn’t popularity contests.
Kierstead January
June 19, 2025 AT 19:05Let’s be real-this whole Lipitor thing is just American medicine’s way of outsourcing responsibility.
You eat like a trash fire? Here’s a pill.
You sit all day? Here’s a pill.
You stress yourself into a coma? Here’s a pill.
Meanwhile, in Japan, people eat fish, walk everywhere, and live to 100 without a single statin.
But no-Americans would rather pay $200 a month than change their diet.
So yes, take your pill.
But don’t pretend you’re healthy.
You’re just medicated.
And that’s not a win.
That’s surrender.