How Hormonal Imbalances Affect Skeletal Muscle Health
Key Takeaways
- Hormones like testosterone, estrogen, cortisol, thyroid hormone, growth hormone and insulin directly shape muscle growth, repair and metabolism.
- Both excess and deficiency can trigger conditions such as sarcopenia, myopathy, cachexia or worsen existing muscular dystrophies.
- Blood tests, muscle strength assessments and imaging are the main tools to spot an endocrine‑muscle mismatch.
- Targeted nutrition, regular resistance training and, when needed, hormone therapy can restore balance and improve function.
- Early detection - especially in aging adults or patients on long‑term steroids - is crucial to prevent permanent loss of muscle mass.
When we talk about skeletal muscle is a type of striated muscle attached to bones that enables voluntary movement, we’re looking at the tissue that makes up most of our body’s mass. Its health isn’t just about strength; it’s a metabolic engine that burns calories, stores glucose and helps regulate hormones themselves. That two‑way street means any hormonal swing can ripple through muscle, and conversely, weak muscles can skew hormone levels.
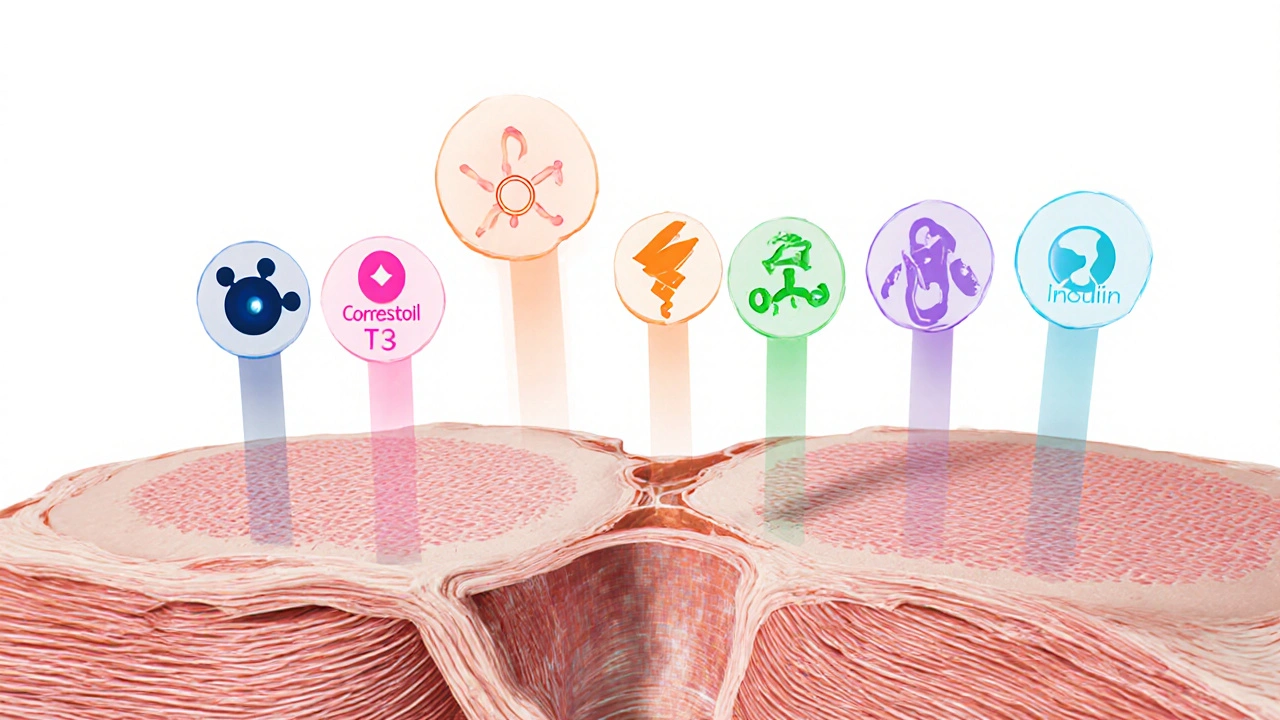
Hormones That Influence Muscle
Several endocrine players have a direct line to muscle cells:
- Testosterone is a male‑dominant androgen that boosts protein synthesis and muscle fiber size. Women produce it too, just at lower levels.
- Estrogen is a female sex hormone that supports muscle repair and influences connective tissue strength.
- Cortisol is a catabolic stress hormone that accelerates protein breakdown when chronically elevated.
- Thyroid hormone (primarily T3 and T4) is a metabolic regulator that determines how fast muscle cells recycle proteins and use energy.
- Growth hormone is a pituitary peptide that stimulates IGF‑1 production, driving muscle growth and repair.
- Insulin is a carbohydrate‑handling hormone that promotes glucose uptake into muscle and curbs breakdown.
How Imbalances Lead to Muscle Conditions
When any of these chemicals drift out of their optimal range, the cascade looks like this:
- Signal disruption: Hormone receptors on muscle fibers either become over‑stimulated (as with excess testosterone) or under‑activated (as with low thyroid).
- Protein synthesis shift: Anabolic hormones (testosterone, IGF‑1) ramp up muscle building; catabolic hormones (cortisol) do the opposite.
- Energy handling change: Insulin resistance forces muscles to rely on fatty acids, which can produce oxidative stress and slow recovery.
- Structural remodeling: Chronic imbalance triggers fibrosis (excess estrogen without proper turnover) or loss of myofibrils (high cortisol).
Over time, these steps translate into recognizable clinical pictures.
Common Muscle Conditions Tied to Hormonal Issues
Sarcopenia
Defined as the age‑related loss of muscle mass and strength, sarcopenia accelerates when testosterone, growth hormone and thyroid hormone decline with age. Studies in the over‑70 population show a 30% faster grip‑strength loss in men with testosterone < 300ng/dL.
Myopathy
Inflammatory or metabolic myopathies often hide an endocrine root. For instance, hyperthyroidism can produce a “thyrotoxic myopathy” where patients feel muscle tremors and weakness despite normal strength tests.
Cachexia
This wasting syndrome, common in cancer or chronic heart failure, is driven by relentless cortisol and inflammatory cytokines that hijack insulin signaling, leading to rapid muscle catabolism.
Muscular Dystrophy Exacerbation
While genetic, the progression of Duchenne or Becker dystrophy can worsen under steroid therapy. Long‑term glucocorticoid use improves inflammation but also raises cortisol, prompting secondary muscle atrophy if not balanced with anabolic support.
Diagnosis and Testing
Pinpointing the endocrine‑muscle link starts with a thorough history and physical exam, followed by targeted labs:
- Serum total and free testosterone (morning draw).
- Estradiol for women and men with unexplained weakness.
- Serum cortisol (AM and PM) to catch diurnal abnormalities.
- TSH, free T3 and free T4 for thyroid status.
- IGF‑1 as a proxy for growth hormone activity.
- Fasting insulin and glucose for insulin resistance assessment.
Muscle assessment tools include hand‑grip dynamometry, a 6‑minute walk test, and, when needed, MRI or ultrasound to visualize fiber quality and intramuscular fat infiltration.
Managing Hormonal Imbalances to Protect Muscle
Intervention blends lifestyle tweaks with medical therapy:
- Resistance training: Proven to boost testosterone, IGF‑1 and insulin sensitivity within weeks. Aim for 2‑3 sessions of compound lifts per week.
- Protein timing: 20‑30g of high‑quality protein (e.g., whey or soy) within 30minutes post‑workout maximizes mTOR signaling, counteracting cortisol effects.
- Sleep hygiene: 7‑9hours reduces nightly cortisol spikes and preserves growth hormone secretion.
- Targeted supplementation: Vitamin D, omega‑3 fatty acids and creatine have modest anabolic effects and improve insulin action.
- Medical correction:
- Testosterone replacement (gel, patches) for clinically low serum levels, monitored for hematocrit and prostate health.
- Levothyroxine for hypothyroidism, titrated to a TSH of 0.5‑2.0mIU/L.
- Cortisol‑sparing strategies: tapering steroids, using mifepristone in Cushing’s syndrome, or adding anabolic agents.
- IGF‑1 analogues in severe growth‑hormone deficiency, prescribed under endocrinology supervision.
Regular follow‑up every 3‑6months helps gauge muscle response via strength tests and hormone panels, allowing dose adjustments before significant loss occurs.

Comparison Table: Hormones vs Their Primary Muscle Effects
| Hormone | Typical Effect on Muscle | Common Imbalance | Resulting Condition |
|---|---|---|---|
| Testosterone | Boosts protein synthesis, increases fiber size | Low (hypogonadism) | Sarcopenia, reduced strength |
| Estrogen | Enhances repair, maintains collagen | Low (menopause) | Muscle fatigue, slower recovery |
| Cortisol | Catabolic, breaks down proteins | High (chronic stress, Cushing’s) | Cachexia, myopathy |
| Thyroid Hormone (T3/T4) | Speeds protein turnover, raises metabolism | Low (hypothyroidism) | Myopathy, sluggish muscle response |
| Growth Hormone / IGF‑1 | Stimulates satellite cell activation | Low (age‑related decline) | Sarcopenia, delayed healing |
| Insulin | Promotes glucose uptake, anti‑catabolic | Resistance (type 2 diabetes) | Accelerated muscle loss |
Next Steps & Troubleshooting
If you suspect a hormone‑muscle mismatch, start with a basic blood panel and a simple strength test (e.g., push‑ups or sit‑to‑stand). Should any result be abnormal, consult an endocrinologist or sports‑medicine physician who can tailor hormone replacement or adjust medication.
Common pitfalls include:
- Self‑prescribing steroids without monitoring cortisol - leads to rapid muscle wasting. \n
- Ignoring nutrition timing - protein after workouts is crucial for using the anabolic window.
- Skipping sleep - even two nights of < 6hours can blunt growth hormone spikes.
Address these early, and you’ll preserve or even regain lost muscle mass while keeping hormones in check.
Frequently Asked Questions
Can low testosterone cause muscle loss in women?
Yes. Although women have lower baseline testosterone, a deficiency can still blunt protein synthesis, leading to reduced strength and slower recovery after exercise.
Why does chronic stress make my muscles feel weak?
Prolonged stress raises cortisol, a hormone that accelerates protein breakdown. Over time, this catabolic environment outweighs the body's ability to rebuild muscle, causing a feeling of weakness.
Is hypothyroidism linked to myopathy?
Absolutely. Low thyroid hormone slows metabolic processes in muscle cells, leading to stiffness, cramps, and a measurable drop in strength - a condition often called hypothyroid myopathy.
Should I get a hormone test before starting a new workout plan?
Not always, but if you notice unexplained fatigue, difficulty gaining strength, or have risk factors (age, chronic illness, steroid use), a basic panel (testosterone, TSH, cortisol) helps tailor your training and nutrition.
Can insulin resistance be reversed to protect muscle?
Yes. Consistent resistance training, a balanced diet low in refined carbs, and adequate sleep improve insulin sensitivity, which in turn reduces muscle protein breakdown.

Kiersten Denton
October 12, 2025 AT 04:54Hormones really are the silent conductors of our muscles.
Michael Vincenzi
October 12, 2025 AT 22:13I've seen how a solid 2‑3 day split of compound lifts can naturally bump testosterone and IGF‑1 within weeks. Pair that with a post‑workout protein shake and you give your muscles the building blocks they crave. Consistency beats intensity; even a modest routine beats sporadic hero sessions. Keep an eye on recovery, because overtraining spikes cortisol, which can undo the gains.
Courage Nguluvhe
October 13, 2025 AT 16:16From a mechanistic standpoint, anabolic signaling cascades such as mTORC1 are exquisitely sensitive to fluctuations in circulating testosterone and insulin. When these hormones dip, the downstream phosphorylation of S6K1 wanes, attenuating myofibrillar protein synthesis. Conversely, hypercortisolemia upregulates FOXO transcription factors, accelerating ubiquitin‑proteasome degradation pathways. Thyroid hormones modulate mitochondrial biogenesis, thereby influencing oxidative capacity and fatigue resistance. Clinically, you can quantify these perturbations via serum assays coupled with dynamometry to construct a composite endocrine‑muscle index. Targeted interventions should therefore be multimodal, integrating endocrine correction with periodized resistance programming.
Oliver Bishop
October 14, 2025 AT 10:20American training programs have been quick to adopt hormone‑optimizing protocols, especially in professional sports where TRT and IGF‑1 analogs are monitored by team physicians. This systematic approach helps keep elite muscle mass on the cutting edge, but it also underscores the need for regular endocrine screening in recreational lifters who push hard. Ignoring the hormonal side can lead to “overtraining syndrome,” where cortisol dominates and performance stalls.
Alissa DeRouchie
October 15, 2025 AT 04:23So like hormones are these crazy little messengers and suddenly you’re all weak? it’s wild how a tiny dip in testosterone can make you feel like you’ve been hitting the gym for years with no results. and cortisol just loves to crash the party when you’re stressed… i guess that’s why sleep matters lol
Emma Howard
October 15, 2025 AT 22:26Remember, every rep you crush is a signal to your body to crank up those anabolic hormones – keep grinding!
dee gillette
October 16, 2025 AT 16:30While the correlation between endocrine status and muscle hypertrophy is evident, causality remains a nuanced, multifactorial construct.
Jasin P.
October 17, 2025 AT 10:33Oh great, another reminder that you can’t out‑lift bad hormones – who would’ve thought?
Lily Đàn bà
October 18, 2025 AT 04:36Honestly, skipping hormone checks is the lazy lifter’s excuse for plateauing; the science isn’t forgiving.
Joseph O'Sullivan
October 18, 2025 AT 22:40Imagine your muscles as a choir; the hormones are the conductor. If the baton wavers, the harmony turns to noise. That’s why balance beats brute force every time.
Conor McCandless
October 19, 2025 AT 16:43When I first stepped into a gym, I believed muscle was forged solely by iron and sweat.
Years of reading research taught me that each lift is also a conversation with a cascade of hormones.
Testosterone, that fierce herald of protein synthesis, whispers to my fibers, urging them to grow.
Estrogen, often dismissed in male narratives, silently repairs micro‑tears and fortifies connective tissue.
Cortisol, the ever‑present stress sentinel, prowls in the shadows, ready to dismantle what you build if recovery is neglected.
Thyroid hormones, the metronome of cellular metabolism, set the tempo for how quickly muscles can recycle proteins.
Growth hormone, released in nocturnal pulses, summons IGF‑1 to awaken satellite cells from dormancy.
Insulin, the humble glucose usher, not only feeds muscles but also guards them against catabolism.
An imbalance in any of these actors can transform a thriving symphony into a discordant cacophony.
Consider the athlete who pushes through endless cardio, only to watch cortisol surge and strength wane.
Or the elder who ignores a dip in testosterone, watching sarcopenia gnaw at independence.
The solution, in my view, lies not in a single magic bullet but in a holistic regimen.
Regular resistance training, timed protein intake, and disciplined sleep collectively orchestrate hormonal harmony.
When you pair that with precise lab monitoring, you can fine‑tune dosages of replacement therapy without veering into excess.
Thus, the path to muscular resilience is paved with science, patience, and the humility to listen to the body's biochemical choir.
kat gee
October 20, 2025 AT 10:46Yeah, those 2‑3 day splits are great – just don’t forget to actually eat the protein, or all that mRNA won’t mean squat.
Courtney Payton
October 21, 2025 AT 04:50Interesting take on the mTOR pathway, but I've seen patients where even with optimal hormone levels, training technique still bottlenecks growth.
Muthukumaran Ramalingam
October 21, 2025 AT 22:53Bro, that whole choir analogy hits different. I always say hormones are like the DJ at a party – if the beats are wrong, nobody dances. In my experience, the biggest mistake is ignoring sleep; you can’t expect GH to drop the mic if you’re snoozing at 3 am. Also, don’t chase supplements blindly; a solid squat rack does more for IGF‑1 than any pre‑workout. Keep the labs in check, but remember the body’s feedback loops are smarter than any spreadsheet. Bottom line: consistency, balance, and a little patience will keep the music playing.
Garrett Williams
October 22, 2025 AT 16:56Exactly, fuel the gains and the results will follow – keep it simple and stay consistent.