Calcium and Iron Supplements: How They Interact with Thyroid Medications

Why Your Calcium and Iron Supplements Might Be Ruining Your Thyroid Medication
If you’re taking levothyroxine for hypothyroidism, and you also take calcium or iron supplements, you might be doing more harm than good-even if you’re doing everything else right. This isn’t a myth. It’s not a rumor. It’s a well-documented, scientifically proven interaction that affects millions of people. And most of them don’t even know it’s happening.
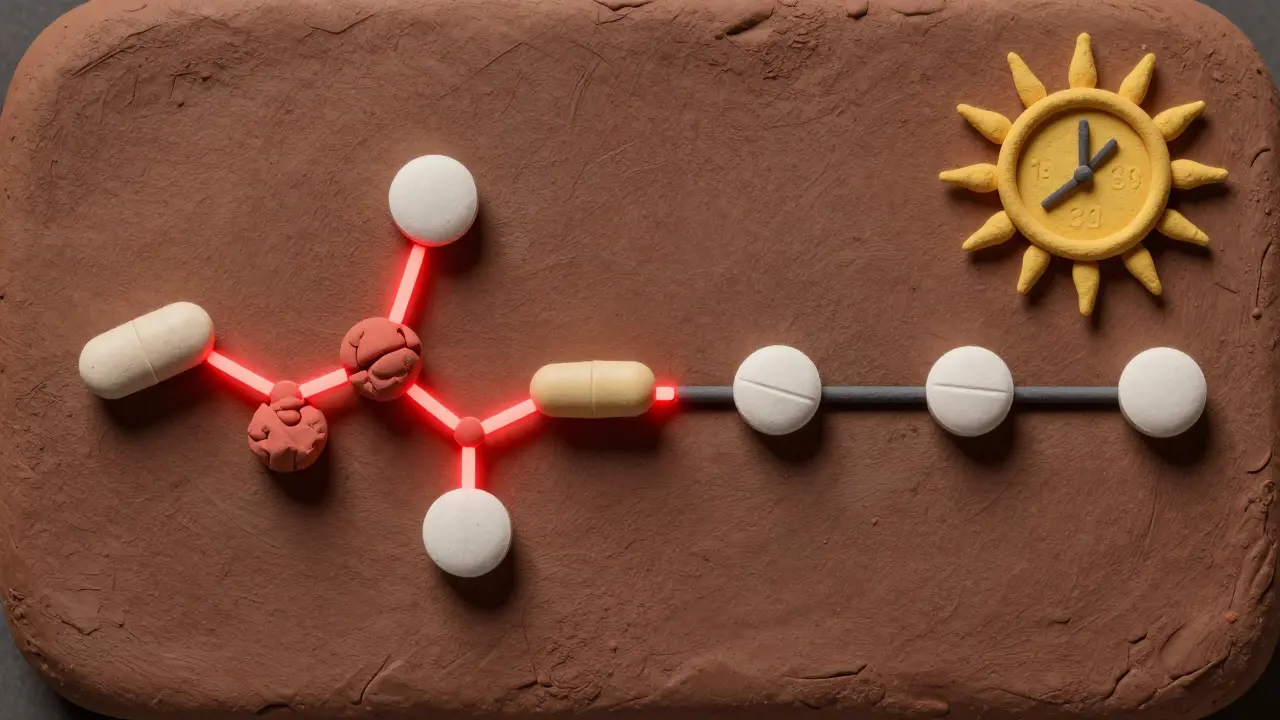
Levothyroxine, the most common thyroid hormone replacement, is absorbed in the small intestine. But calcium and iron? They bind to it like glue. Together, they form a chemical compound your body can’t absorb. That means your thyroid medication isn’t working. Your TSH levels rise. Your fatigue gets worse. Your weight creeps up. You feel like you’re back at square one-when you thought you were finally getting control.
How Much Do They Really Interfere?
It’s not a small effect. A 2000 study published in the Journal of Clinical Endocrinology & Metabolism found that taking just 1,200 mg of calcium carbonate (about the amount in two Tums tablets) at the same time as levothyroxine reduced absorption by 22% to 36%. Another study in 2008 showed that a single 325 mg iron pill (ferrous sulfate) dropped absorption by 21%. That’s not a little bump-it’s a crash.
And it’s not just pills. Calcium-fortified orange juice? One 8-ounce glass has around 350 mg of calcium. If you drink it with your thyroid med, you’re cutting its effectiveness by nearly a third. Same with iron-fortified cereals or protein bars. Even if you take your thyroid pill in the morning and your supplement at lunch, you might still be in the danger zone.
The American Association of Clinical Endocrinologists says iron supplements taken within two hours of levothyroxine can reduce absorption by up to 39%. That’s not a typo. Nearly 4 out of 10 doses wasted. And the worst part? You won’t feel it right away. Your doctor won’t notice it until your next blood test-maybe months later-when your TSH is suddenly sky-high and you’re told, “Your dose needs to go up.” But it’s not your dose. It’s your timing.
What Happens When You Don’t Separate Them
Imagine this: You’ve been on levothyroxine for a year. You feel good. Your energy’s back. Then you start taking a prenatal vitamin with iron because you’re pregnant. Or you get diagnosed with osteoporosis and your doctor prescribes calcium. A few months later, you’re tired again. Your hair’s falling out. You’re cold all the time. You think it’s stress. Or aging. Or maybe your meds aren’t working anymore.
But it’s not that. A 2017 study of 450 patients found that 4.4% developed TSH levels above 5 mU/L within a year after starting calcium supplements without proper separation. That’s clinically significant. And in pregnant women, the stakes are even higher. One case study showed a woman taking iron just four hours after her thyroid pill still had a TSH of 8.2 mU/L-way above normal-and low thyroid hormone levels. She needed a dosage increase just because the timing was off.
And it’s not just calcium and iron. Soy milk, walnuts, high-fiber meals, coffee, grapefruit juice, even biotin supplements can interfere. But calcium and iron are the biggest culprits because they’re so common. One in five adults over 50 takes calcium. One in three women of childbearing age takes iron. And most of them are also on thyroid meds.
How to Take Them Right: The Real Timing Rules
Let’s cut through the confusion. Here’s what actually works, based on guidelines from the American Thyroid Association, Mayo Clinic, and the European Thyroid Association.
- Take your thyroid medication on an empty stomach. First thing in the morning, with a full glass of water. Wait at least 30 to 60 minutes before eating, drinking coffee, or having anything else.
- Wait four hours before taking calcium. This is the gold standard. Mayo Clinic, Synthroid’s manufacturer, and the American College of Endocrinology all say four hours. That means if you take your thyroid pill at 7 a.m., don’t take calcium until 11 a.m. or later.
- Wait two to four hours before taking iron. Some guidelines say two hours, others say four. When in doubt, go with four. Iron is especially tricky because it’s often taken at night for stomach comfort-but that’s the worst time if you’re on thyroid meds. If you take iron at night, make sure your thyroid pill was taken at least four hours before bedtime.
- Don’t take them together. Not even 15 minutes apart. Not even if you think you’re being careful. The binding happens fast.
Some people find it easier to take their thyroid pill at bedtime-after dinner, at least four hours after the last meal. That way, they can take calcium or iron with dinner without conflict. A 2022 Reddit thread from a user named u/HypoMama described how switching to nighttime levothyroxine fixed her iron-related absorption issues after postpartum anemia. Her TSH dropped from 7.1 to 2.3 in three months.
What About the Newer Thyroid Medications?
There’s some hope on the horizon. In March 2023, a study in the Journal of Clinical Medicine tested a new liquid formulation of levothyroxine. When taken with calcium, it only lost 8% absorption-compared to 32% for the standard tablet. That’s a game-changer. But here’s the catch: it costs about $350 a month. Generic levothyroxine? Around $15.
Until these new forms become affordable and widely available, the old rules still apply. And they’re not going away. Even if you switch brands-from Synthroid to Tirosint or NP Thyroid-the interaction with calcium and iron stays the same. The active ingredient is still levothyroxine. The binding doesn’t care what brand name is on the bottle.
Who’s Most at Risk?
You’re more likely to run into this problem if you’re:
- A woman over 50 (higher risk for osteoporosis and hypothyroidism)
- Pregnant or postpartum (iron needs spike)
- Menopausal (calcium and thyroid issues often overlap)
- On multiple medications (especially for heart disease, diabetes, or anemia)
- Over 65 (slower digestion means longer exposure to binding agents)
And here’s the kicker: a 2023 study in the Journal of the American Board of Family Medicine found that only 42% of patients got proper counseling about supplement interactions when they first started thyroid medication. Most doctors assume patients know. Most patients assume it’s fine. And so the problem grows.

What Else Can Interfere?
Calcium and iron aren’t the only troublemakers:
- Soy products (tofu, soy milk, edamame): Can increase your levothyroxine dose by 18-30%
- Walnuts: Reduce absorption by 24% if eaten with your pill
- Coffee and tea: Tannins interfere. Wait at least 60 minutes after taking your pill
- High-fiber foods (oats, beans, bran): More than 30g of fiber within an hour of your dose can raise TSH by 15-25%
- Biotin: At doses over 5 mg daily, it can trick lab tests into showing fake high thyroid levels. Don’t take it for hair or nails unless you’ve talked to your doctor.
It’s not about being perfect. It’s about being aware. You don’t have to give up your smoothie or your multivitamin. You just need to move them to a different time of day.
What to Do If You’ve Been Taking Them Together
If you’ve been taking calcium or iron with your thyroid pill for months-or years-here’s what to do:
- Don’t panic. Your thyroid isn’t permanently damaged.
- Don’t stop your meds. That’s dangerous.
- Don’t change your dose on your own. Your doctor needs to adjust it based on blood work.
- Start separating them now. Follow the four-hour rule for calcium, four hours for iron.
- Ask for a TSH and free T4 test in 6 to 8 weeks. That’s how long it takes for your levels to stabilize after changing timing.
Many patients see their TSH drop back into range within two months once they fix the timing. No dose change needed. Just better timing.
The Bottom Line
Thyroid medication works when it’s absorbed. Calcium and iron block that absorption. It’s simple chemistry. And it’s preventable.
You don’t need to be a scientist to get this right. Just remember: thyroid pill first thing in the morning, water only, wait an hour. Then wait four hours before you take calcium or iron. If you take your thyroid pill at night, make sure it’s been four hours since your last meal and your last supplement.
It’s not about perfection. It’s about consistency. And if you’re taking multiple meds, write it down. Set alarms. Use a pill organizer with time slots. Your body will thank you.
And if your doctor hasn’t told you this? Tell them. Because this isn’t just a tip-it’s a medical necessity. Millions of people are getting the wrong dose because of something as simple as when they took their supplement. You don’t have to be one of them.
Can I take calcium and iron together with my thyroid medication if I space them out?
No. Even if you take calcium first, then iron an hour later, both will still bind to your thyroid medication if it’s still in your stomach or upper intestine. The safest approach is to separate both supplements by at least four hours from your thyroid pill. Don’t stack them. Space them out completely.
What if I forget and take them together? Do I need to retake my thyroid pill?
No, don’t retake your thyroid medication. Taking a double dose can cause symptoms of hyperthyroidism-racing heart, anxiety, tremors. Instead, skip the next dose of your supplement and go back to your regular schedule. Don’t try to make up for it. Just get back on track. Your body will adjust. Talk to your doctor about getting your TSH checked in 6 to 8 weeks.
Is there a better time of day to take calcium and iron?
Yes. For calcium, take it with dinner or right before bed-after your thyroid pill has had time to absorb. For iron, many people take it at night anyway because it can upset the stomach. If you take your thyroid pill in the morning, nighttime iron is ideal. If you take your thyroid pill at night, take iron in the afternoon-never within four hours of your thyroid dose.
Do all forms of calcium and iron interfere the same way?
Yes. Calcium carbonate, calcium citrate, ferrous sulfate, ferrous fumarate, ferrous gluconate-all of them interfere. The cations (calcium and iron ions) are what bind to the medication, not the form they’re in. So whether it’s a tablet, chewable, gummy, or liquid, the interaction still happens. The only exception might be newer formulations like liquid levothyroxine, but those aren’t widely available yet.
Can I get enough calcium and iron from food without supplements?
For calcium, yes-dairy, leafy greens, canned fish with bones, and fortified plant milks (if you take them at the right time) can help. For iron, red meat, lentils, spinach, and fortified cereals work, but non-heme iron (from plants) is harder to absorb. If you’re anemic, you might still need supplements. Just make sure to time them correctly. Food is safer than pills, but timing still matters.
Why do some doctors say two hours is enough?
Some guidelines, like the European Thyroid Association, suggest two to three hours for iron. But the American guidelines are stricter. Why? Because individual digestion varies. Some people absorb meds faster. Others slower. If you’re over 65, pregnant, or have gut issues, your absorption window is longer. Four hours is the safest buffer. If your doctor says two hours, ask them to explain why-especially if your TSH keeps rising.
Should I stop taking calcium or iron altogether?
No. Calcium is critical for bone health, especially after menopause. Iron is essential for oxygen transport, especially during pregnancy or heavy periods. The goal isn’t to quit supplements-it’s to take them at the right time. You can still get all the benefits without sabotaging your thyroid treatment.

June Richards
February 1, 2026 AT 03:39Jaden Green
February 1, 2026 AT 14:33Lu Gao
February 3, 2026 AT 02:13Nicki Aries
February 3, 2026 AT 22:53Lilliana Lowe
February 5, 2026 AT 03:32vivian papadatu
February 6, 2026 AT 21:28Bryan Coleman
February 7, 2026 AT 13:20Naresh L
February 7, 2026 AT 21:48Sami Sahil
February 8, 2026 AT 14:44Bob Cohen
February 10, 2026 AT 12:48Nidhi Rajpara
February 11, 2026 AT 10:58Melissa Melville
February 12, 2026 AT 11:38Nancy Nino
February 12, 2026 AT 21:16