Bioavailability Studies for Generics: What They Test and Why It Matters for FDA Approval
What bioavailability studies actually measure in generic drugs
When you pick up a generic pill at the pharmacy, you might assume it’s just a cheaper copy of the brand-name version. But behind that simple swap is a complex science called bioavailability testing. These studies don’t just check if the generic has the same active ingredient-they prove it behaves the same way inside your body.
Bioavailability means how much and how fast a drug gets into your bloodstream after you take it. For generics, regulators like the FDA require two key numbers: AUC (Area Under the Curve) and Cmax (Maximum Concentration). AUC tells you the total amount of drug absorbed over time. Cmax shows how high the drug spikes in your blood. Together, they answer: does this generic deliver the same drug, at the same rate, in the same amount?
It’s not enough for the generic to contain the same chemical. A pill made with different fillers, coatings, or manufacturing methods might dissolve too slowly or too fast. That changes how your body absorbs it. A bioavailability study catches those differences before the drug ever reaches shelves.
Why the 80-125% rule exists-and why it works
The FDA doesn’t demand that generics match brand-name drugs exactly. Instead, they use a range: the 90% confidence interval for AUC and Cmax must fall between 80% and 125%. That means the generic can be 20% lower or 25% higher in absorption and still be approved.
That range isn’t random. It’s based on decades of clinical data showing that a difference this small rarely affects how well a drug works or how safe it is. For most medications, a 10% variation in blood levels won’t change your outcome. Think of it like driving: if your car’s speedometer reads 60 mph but you’re actually going 55 or 65, you’re still in the same legal zone.
But for drugs with a narrow therapeutic index-like warfarin, digoxin, or levothyroxine-the rules tighten. Here, the acceptable range shrinks to 90-111%. These drugs have a small margin between helping you and harming you. Even a small shift in absorption can trigger side effects or reduce effectiveness. That’s why doctors sometimes prefer to keep patients on the same brand for these.
How bioequivalence studies are done (and why healthy volunteers are used)
Most bioequivalence studies happen in clinical research units with 24 to 36 healthy adults. Why healthy? Because researchers need to isolate how the drug behaves without interference from disease, other medications, or organ damage.
The design is usually a crossover study: each volunteer takes the brand-name drug in one period, then the generic in another, with a washout period in between-long enough for the first drug to fully leave the body. This cuts down on individual differences. One person might naturally absorb drugs faster than another. By testing them on both, you compare apples to apples.
Blood samples are drawn every 15 to 60 minutes over 24 to 72 hours, depending on how long the drug lasts. Labs then measure the drug concentration using highly sensitive instruments. The data gets plotted into curves, AUC and Cmax are calculated, and statistical tests confirm whether the generic falls within the 80-125% range.
It’s expensive. A single study can cost $200,000 to $500,000. That’s why companies only run them when they’re ready to submit an application to the FDA. Over 1,200 of these studies are done globally every year.
When bioequivalence studies aren’t needed (and why)
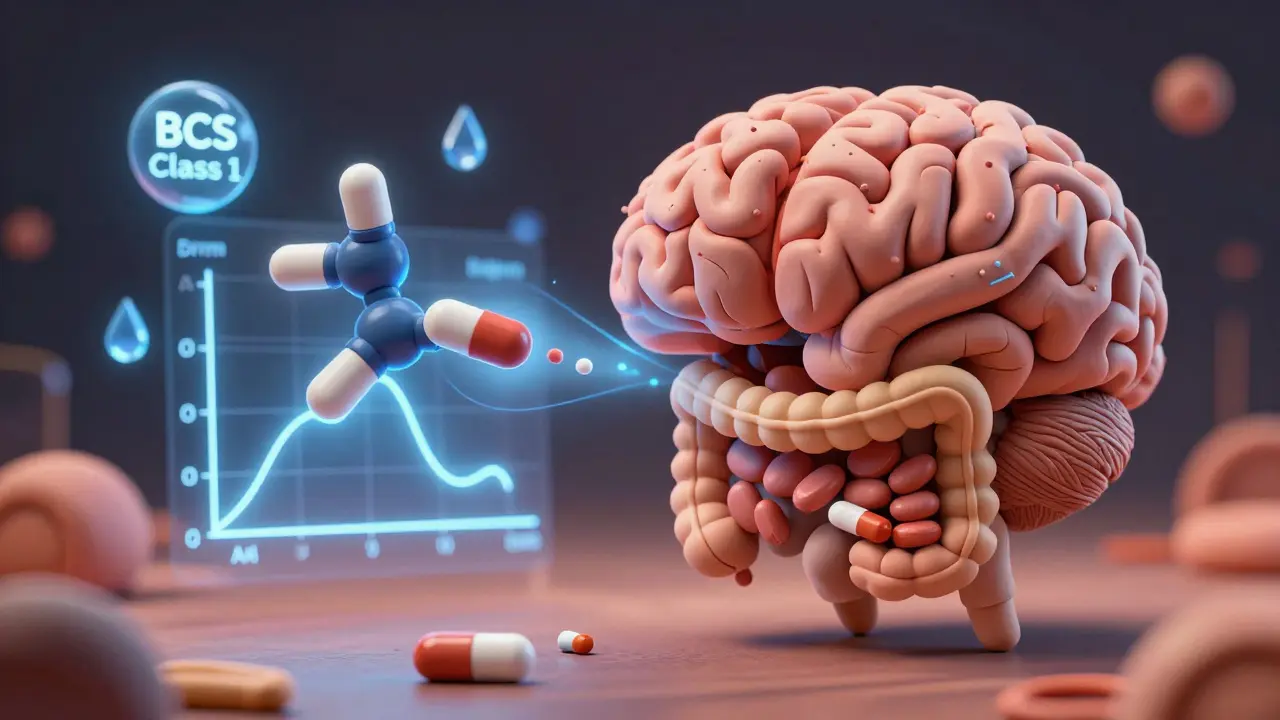
Not every generic needs a full human study. The FDA allows waivers under the Biopharmaceutics Classification System (BCS). If a drug is:
- Highly soluble in water
- Highly permeable through the gut wall
- Dissolves quickly in the stomach
then it’s classified as BCS Class 1. For these, the FDA accepts in vitro tests-like dissolving the pill in lab fluid-instead of blood draws. About 30% of approved generics qualify for this shortcut.
BCS Class 3 drugs (high solubility, low permeability) can also qualify if the formulation matches the brand-name exactly. This saves time and money without risking patient safety. The science behind it is solid: if the drug dissolves and absorbs predictably, and the ingredients are identical, then human testing adds little new value.
Where the system breaks down-and what’s being done about it
For simple pills, the bioequivalence system works incredibly well. But for complex products, it’s not perfect. Think of extended-release capsules, inhalers, gels, or injectables. These don’t just release the drug-they control how it’s released over hours. A generic might release the same total amount, but too slowly at first or too fast later.
That’s why the FDA has issued 11 new product-specific guidelines since 2023 for tricky drugs like testosterone gel, budesonide inhalers, and topical antifungals. These require extra testing: multiple time points, different endpoints, or even skin irritation measurements instead of blood levels.
Highly variable drugs-like tacrolimus or clopidogrel-are another challenge. Some people absorb them wildly differently. For these, the FDA now uses scaled bioequivalence (RSABE), which adjusts the acceptance range based on how much the drug varies from person to person. If the brand itself swings a lot, the generic can swing too, as long as it matches the brand’s pattern.
Real-world impact: Do generics really work like the brand?
Patients sometimes report feeling different after switching. A cardiologist might see a few cases where a patient developed palpitations after switching from brand-name amlodipine to generic. But these are rare. Out of thousands of patients, it’s less than 0.1%.
Meanwhile, pharmacists who’ve run hundreds of bioequivalence studies report no differences in real-world performance once the drug passes FDA standards. The Generic Pharmaceutical Association says 90% of patients can’t tell the difference between brand and generic in terms of effectiveness.
Even in sensitive areas like epilepsy, where patients worry about seizure control, the FDA found only 6.4% of reported issues after generic switches were linked to bioequivalence problems. The rest were due to missed doses, stress, or other factors.
What’s clear: if a generic passes FDA bioequivalence testing, it’s as safe and effective as the brand for the vast majority of people.
The future: AI, modeling, and smarter testing
The next big shift isn’t more blood draws-it’s less. The FDA is now using artificial intelligence to predict how a generic will behave based on its ingredients and manufacturing process. In a 2023 pilot with MIT, machine learning predicted AUC ratios with 87% accuracy across 150 drugs.
Model-informed drug development (MIDD) lets companies use computer simulations to reduce the number of human subjects needed. If a drug’s absorption pattern is well understood, you might only need 12 volunteers instead of 36.
These tools won’t replace testing entirely. But they’ll make it faster, cheaper, and more precise-especially for complex drugs that used to take years to approve. The goal? Get safe, affordable generics to market faster without cutting corners.
Why this matters for you
Generics save the U.S. healthcare system over $300 billion a year. Without bioequivalence studies, we wouldn’t have them. These tests ensure that when you pay less, you’re not getting less. The system isn’t perfect, but it’s grounded in real science-not guesswork.
If you’ve had a bad experience after switching, talk to your doctor. But know this: the odds are overwhelmingly in favor of the generic working just as well. The FDA’s system has protected millions of patients for over 40 years. And it’s still getting smarter.

mike swinchoski
January 13, 2026 AT 04:54jefferson fernandes
January 14, 2026 AT 21:22Acacia Hendrix
January 16, 2026 AT 06:56James Castner
January 17, 2026 AT 05:50Adam Rivera
January 17, 2026 AT 22:19Rosalee Vanness
January 18, 2026 AT 05:08lucy cooke
January 19, 2026 AT 08:33Trevor Davis
January 20, 2026 AT 06:47